Boost Your Brain (40 page)
Authors: Majid Fotuhi

If Sara’s doctors didn’t find specific evidence of the cause of her dementia, she would likely be diagnosed with
Alzheimer’s disease,
a subset or type of dementia (although people often use the terms dementia and Alzheimer’s interchangeably). With Alzheimer’s, as with many other forms of dementia, Sara might experience profound memory and cognitive problems as well as personality and behavioral changes. She might get lost in her own neighborhood, forget how to tie a shoelace, or be unable to operate a simple device like a can opener. She might be sad for no reason, or cry or fly into a rage without provocation. Though she might remain physically healthy, Alzheimer’s is a progressive, degenerative disease, so it inevitably worsens and leads to death. If her brain were examined after her death, it would likely be full of amyloid plaques and tau tangles, the hallmark toxic protein clumps of Alzheimer’s disease.
To illustrate the difference between memory deficits seen in normal aging, mild cognitive impairment, and Alzheimer’s disease, we can think about what might happen a few days after one of those parties I attend.
If I were to bump into a person with benign age-related memory problems and ask “who did you talk to at the party last weekend?” I might get a response along the lines of “I spent a lot of time with that woman I always see in the lunch room at work. She’s tall, blonde, and very friendly. I know she told me, but I can’t remember her name.”
A person with mild cognitive impairment, on the other hand, might say, “I talked to so many people. I just have no idea who!”
A person with Alzheimer’s, though, would have a strikingly different answer. When asked about the party they’d attended just a few days before, this person might look genuinely perplexed and pose a question of her own: “What party?”
What Causes Alzheimer’s
As telling as the “what party?” response is, it doesn’t actually identify for us specifically what’s going on inside the brain of the sufferer. “What party?” tells us there’s a problem but not why it occurred.
So, why
does
Alzheimer’s occur? The answer depends on what you mean by Alzheimer’s. There are actually two distinct types of Alzheimer’s: early-onset and late-onset.
In early-onset Alzheimer’s disease, which often strikes people in their fifties and sixties, we know exactly what causes the brain shrinkage and decline associated with the condition. Alzheimer’s pathology—amyloid plaques and tau tangles—wreak havoc, rapidly killing brain cells. And while plaques and tangles don’t show up on commonly used brain scans, brain MRIs of early-onset Alzheimer’s patients do show marked atrophy in the hippocampus in the early stages, followed by atrophy scattered throughout the brain. I think of it as a forest fire. The match may be dropped in the hippocampus, but the flames quickly spread—with devastating results.
You might consider early-onset Alzheimer’s a “pure” form of the disease because it has solely Alzheimer’s pathology, rather than the consequences of lifestyle factors or medical conditions, at its root. This form of the disease is largely determined by genetic makeup and it accounts for a small subset of total Alzheimer’s cases. How small? In the United States an estimated two hundred thousand people have early-onset Alzheimer’s.
2
Given that about five million people have Alzheimer’s disease, we can assume the portion of those having early-onset Alzheimer’s is about 4 percent.
The other 96 percent have late-life Alzheimer’s disease. The brains of these people exhibit the same shrinkage in the hippocampus and across the brain, but they also often harbor clues pointing to other causes. In fact, in the brains of people who develop Alzheimer’s disease in late life we often see signs of both silent strokes and atrophy caused by other neurodegenerative conditions, such as Lewy body disease, as well as any number of health problems—obstructive sleep apnea, hypertension, diabetes, and depression, to name a few.
3
In contrast to early-onset Alzheimer’s disease, in late-life Alzheimer’s disease genetics make up a small part of the risk. To put that genetic contribution into perspective, consider this: while the average seventy-year-old man has a roughly 2 percent chance of developing late-life Alzheimer’s disease, someone of the same age who has close relatives with late-life Alzheimer’s might have a 4 percent chance. That’s double the chance, sure, but just like buying two lottery tickets instead of one doubles your likelihood of winning (but still leaves you highly unlikely to walk away with millions), doubling your risk of Alzheimer’s disease at this level is hardly a death knell.
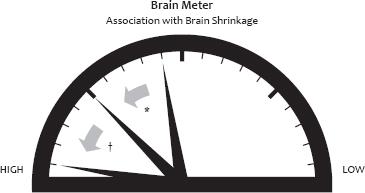
A far larger portion of the risk of developing late-life Alzheimer’s disease is tied to a group of factors we have some degree of control over. Give that seventy-year-old multiple vascular risk factors, such as high blood pressure, a BMI greater than 30, physical inactivity, and high total cholesterol, and his risk of developing late-life Alzheimer’s disease rockets to 32 percent.
4
Many studies have examined the link between clinical symptoms of dementia and the primary pathology in the brain.
5
In one—with the telling title “Mixed Brain Pathologies Account for Most Dementia Cases in Community-Dwelling Older Persons”—researchers at Chicago’s Rush University Medical Center carefully examined the brains of 141 deceased elderly people and came to the conclusion that many did not have just a single abnormality.
6
The most common abnormality the research team noted was a mix of plaques, tangles, small strokes, large strokes, and Lewy bodies (Parkinson’s-like lesions). In fact, those with dementia had a load of plaques and tangles similar to those without dementia; what was different was the presence of other pathological components in what I call a “soup of factors.” Thus, the best diagnosis for such patients would be “mixed dementia,” although in most cases they are instead labeled as having Alzheimer’s disease.
In
chapter 16
, I’ll address the controversy over terminology surrounding late-life Alzheimer’s disease. But for now it’s enough to know that when it comes to dementia that strikes in late life I consider Alzheimer’s pathology yet another brain-shrinking factor, one among the soup of other factors, such as diabetes, obesity, stroke, TBI, alcohol abuse, stress, poor sleep, and depression.
The Tricky Business of Diagnosis: Silent Alzheimer’s
Though we have amassed an impressive array of technologies related to the brain, we still don’t have a simple, reliable, and definitive method of determining if someone has Alzheimer’s disease. Unlike diabetes, which we can detect through a blood test, or hypertension, which we identify through blood pressure readings, there is no single test for Alzheimer’s disease.
Often diagnosis, then, is tricky. This is less true in the case of “pure” early-onset Alzheimer’s disease, which tends to be fairly straightforward. Patients who develop dementia in their fifties and sixties often experience a rapid decline in their memories and ability to function without signs of the soup of other factors—a tip-off that Alzheimer’s might be the sole cause.
By contrast, late-onset Alzheimer’s patients tend to see their cognitive decline progress more slowly and their neurological evaluations often turn up hints of other conditions—like vascular disease—that contribute to shrinkage in the brain. Making diagnosis more difficult, this soup of brain shrinkers varies in every person. Some may have a few ingredients; others may have many. The evidence may be clear (like a major stroke) or almost invisible (like thousands of micro strokes).
Until fairly recently, the only way to confirm Alzheimer’s disease was by examining the brain after death. If the person suffered from dementia while alive and had an accumulation of plaques and tangles in the brain, that person would have a confirmed case of Alzheimer’s disease. But even then there was, and still is, room for variation. Some doctors make their diagnoses based solely on the prevalence of amyloid plaques; some consider amyloid plaques and tau tangles; still others give tau tangles the lion’s share of the weight. There is no single “gold standard” in diagnosing Alzheimer’s (even after death), which, as you can imagine, leads to great discrepancies in who is diagnosed and with what.
7
Even Alzheimer’s experts in academic centers may have different opinions when it comes to diagnosis. I experienced this firsthand in the early 2000s when I was a consultant for the Johns Hopkins Alzheimer’s Disease Research Center, which convened weekly meetings with a group of neurologists, psychiatrists, and pathologists. Together we would discuss patients who, after being monitored for twenty or thirty years, had recently died. Hearing about their symptoms and test results, we’d each make an educated guess as to their diagnoses, based on the pathological findings. Was it mild cognitive impairment? Alzheimer’s? Lewy body dementia? Vascular dementia? In many cases, individual members of the team disagreed on the diagnoses. Although that was a decade ago, the lack of consensus among experts persists, despite the aid of improved technologies.
Such discrepancies may be, in part, because some elderly people have “silent” Alzheimer’s in their brains. Just as silent strokes can cause damage without leading to symptoms, “silent” Alzheimer’s pathology—those plaques and tangles—can also do harm without leading to noticeable symptoms. It’s only when combined with other factors that a threshold is reached and cognitive decline begins.
This might explain why the Alzheimer’s
pathology
we’ve long associated with Alzheimer’s disease doesn’t always correlate well with late-life Alzheimer’s
symptoms.
Some people have Alzheimer’s plaques and tangles and never develop symptoms, while others have the same load of pathology and become demented. Why? The reason likely has to do with the co-existence of silent strokes, concussions, or medical conditions as well as the strength of the person’s brain reserve. Each brain shrinker chips away at the brain’s buffer; when multiple shrinkers are combined, the deficits overcome the brain reserve.
One often-cited piece of evidence for this is the so-called Nun Study, which began in the 1980s and followed the health and lifestyle of 678 American members of the School Sisters of Notre Dame.
8
At its heart, the study aimed to answer the question of why some elderly people suffer from dementia while others do not. What was their secret? How did the über-sharp ninetysomethings among us do it? The nuns, it was hoped, would offer an answer.
As part of the study, participants agreed to have their brains examined after they died. When considered along with detailed cognitive studies and MRIs taken while the nuns were alive, the autopsied brains offered up some surprising clues. Nuns whose brains had Alzheimer’s tau tangles but no sign of strokes typically hadn’t displayed any outward symptoms of Alzheimer’s disease while they were alive. Similarly, many of those who’d had multiple strokes—large or small—but few tangles in their brains did not show symptoms of Alzheimer’s disease. But those who had tangles
and
evidence of strokes had a strong likelihood of displaying Alzheimer’s symptoms. Alzheimer’s pathology, it seemed, wasn’t the sole cause of late-life Alzheimer’s disease for most nuns in the study.
Given that symptoms likely reflected a mix of factors, which do you blame? Should we point the finger at tangles? Or silent strokes? Or were there other factors too?
Does it really matter what we call it? Actually, it does, as the loved ones of any recently diagnosed Alzheimer’s sufferer would tell you. Alzheimer’s disease is often seen as heartbreakingly unalterable—a death sentence.
I often favor using the term “mixed dementia” in cases where I believe multiple etiologies have contributed to a patient’s decline. This would help to ensure that only those whose Alzheimer’s symptoms are caused primarily by Alzheimer’s pathology would be diagnosed as having Alzheimer’s disease.
Such a distinction has a benefit beyond just the impact on patients. In research studies, focusing just on patients who have significant plaques and tangles—and excluding those whose dementia had other causes—would allow scientists to be more targeted than ever. An amyloid-busting drug would offer little benefit to someone whose dementia was 80 percent stroke-related and only 20 percent caused by plaques and tangles, for example. Removing that person from the Alzheimer’s disease category would allow researchers to instead study just those who might benefit from amyloid removal. In fact, this may be the key reason that all the amyloid-busting drugs have failed so far: they’ve been tested on too broad a group.
The plaques and tangles of Alzheimer’s Disease, especially in young patients, can rapidly destroy the brain.