i bc27f85be50b71b1 (208 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

Numerous etiologies of SIADH exist, with the most frequent cause
being small cell or oat cell carcinomas of the lung. Other etiologies
include the following'·15:

666
AClITE CARE HANDBOOK FOR PIIYSICAL THERAPISTS
• Bacterial pneumonias, chronic obstructive pulmonary disease,
tuberculosis, lung abscesses
• Malignancies of the pancreas, duodenum, colon, lymphoid tissue, and thymus
• Medication side effects from anti psychotics, sedative-hypnotics,
diuretics, antihypertensives, analgesics, cardiac drugs, and antibiotics
• Head trauma, cenrral nervous system neoplasms
A mild condition of SlADH is usually asymptomatic. More severe
cases, however, can result in fluid and electrolyte imbalances, resulting
in interstitial edema from a lack of serum sodium. Many systems will
be affected by this edema, with the nervous system being most severely
involved. Manifestations can include any of the following: headaches,
nausea, confusion, increased blood pressure, peripheral edema, and
cerebral edema that leads to seizures and coma (in severe cases).l5
Management of SIADH may consist of any of the following: treatment of the underlying cause, fluid restriction, intravenous administration of sodium chloride solution, or administration of diuretics (furosemide).l5
Clinical Tip
The physical therapist should be aware of fluid restriction
guidelines for patients with SIADH, especially because
activity during physical therapy may increase the patient's
thirst. These guidelines are often posted at the patient's
bedside.
Hypopituitarism
There are numerous causes for primary (pituitary directly affected) or
secondary (hypothalamus or pituitary stalk affected) hypopituitarism.
The most common causes of primary hypopituiatarism are piruitary
neoplasms, such as pituitary adenomas and craniopharyngioma, and
ischemic necrosis occurring during the late stages of pregnancy (Sheehan's syndrome). Common causes of secondary hypopituitarism include hypothalamic tumors, cranial trauma, sarcoidosis, surgical
destruction of the pituitary stalk, or a combination of these.6•lJ,16.17
ENDDCR[NE SYSTEM
667
Symproms, physical findings, and management depend on the
extent of the disorder and the specific hormone and target cells
involved. Patients with complete pituitary hormone deficiency (panhypopituitarism) present with the following",[6:
• Hypogonadism
• Amenorrhea, regression of secondary sexual characteristics, and
infertility
• Dilutional hyponatremia
• Diabetes insipidus (OI)
• Short stature (in children)
• Hypothyroidism
• Glucocorticoid deficiency
Management of panhypopituitarism may consist of any of the following: replacement therapy or pituitary hormones, such as thyroxine, glucocorticoids, and GH for children; desmopressin for 01; androgen therapy for men; or estrogen therapy for women younger
than SO years of age. Management of other clinical sequelae of
hypopituitarism will be specific ro the involved areas.'I,[6
Diabetes Insipidus
01 involves the excretion of a large volume (i.e., greater than 30
ml/kg per day) of dilute urine (hyporonic polyuria). 01 may result
from hypothalamic, pituitary, renal, or psychogenic disorders;
however, most incidences of DI are described as idiopathic,6.ls
Piwirary DI involves the failure to synthesize or release vasopressin (AOH). Renal, or nephrogenic, OJ is a deficiency of vasopressin receptors in the renal collecting ducts. Psychogenic or dipsogenic OJ involves a large intake of fluid that may suppress
ADH secrcrion.7·8•1I,18
Signs and symproms of OJ may be transient or permanent and
include the following7,8,[6.[8:
• Polyuria, nocruria
• Thirst (especially for cold or iced drinks), polydipsia


668
AClTfE CARE HANDBOOK FOR PHYSICAL THERAPISTS
• Dehydrarion
• Weighr loss
• Dry skin with decreased turgor
• Central nervous system manifestations (e.g., irritability, mental
dullness, ataxia, hyperthermia, and coma) if access to water is
interrupted
Management of neurogenic (hypothalamic or pituitary dysfunction)
Dl may consist of pharmacologic treatment, such as the following:
aqueous vasopressin or deamino-8-D-arginine vasopressin (Desmopressin), chlorpropamide (Diabinase), and clofibrate (Atromid-S).
Management of nephrogenic (renal) 01 may consist of diuretics
such as hydrochlorothiazide (HydroDIURIL), in combination with a
sodium-restricted diet.7·8•19
Adrenal Gland
Function
The adrenal gland has two distinct areas, the outer correx and the
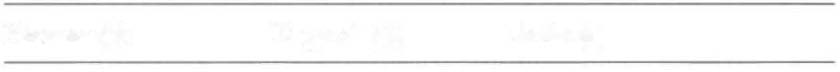
inner medulla, that differ in their function and embryologic origin.- Table 11-7 summarizes the target sites and actions of the adrenal gland.
Adrenal and Metabolic Tests
Adrenal Tests
Evaluation of the adrenal cortical (glucocorricoids, androgens, and
mineralocorticoids) and medullary (epinephrine and norepinephrine)
hormones is described below. Anatomic investigation of the adrenal
glands may also be performed to diagnose possible adrenal dysfunction. Common methods to accomplish this are computed tomography scan (to identify adrenal tumors), radioisotope scan using seleno-cholesterol, ultrasound, arteriogram, adrenal venogram (allows measurements of hormone levels), and intravenous pyelogram (see Diagnostic Tests in Chapter 9).",20

ENDOCRINE SYSTE..\1
669
Table 1 1-7. Target Sites and Actions of Adrenal Gland Hormones
Hormone(s)
Target site(s)
Action(s)
Cortex
Mineralocorticoids
Kidney
Reabsorption of sodium and
(aldosterone)
water
Elimination of potassium
Glucocorticoids
Systemic
Metabolism of carbohydrate,
(cortisol)
protein, and fat
Response to stress
Suppresses immune responses
Anti-inflammarion
Sex hormones
Systemic
Preadolescent growth spurt,
(androgens.
affects secondary sex charprogesterone,
acteristics
and estrogen)
Medulla
Epinephrine
Cardiac and
Emergency functions
smooth muscle,
Stimulates the action of the
glands
sympathetic system
Norepinephrine
Organs innervated
Chemical transmitter subby sympathetic
stance
nervous system
Increases peripheral resistance
Sources: Data (rom BF Ful er. Anatomy and Physiology of the Endocrine System. In CM
Hudak, BM Gallo (cds), Critical Cllfe Nursing: A Holistic Approach (6th ed). Philadelphia:
Uppincort, 1994;875; and JV Corbcn (ed). L'lboratory Tests and Diagnostic Procedures
with Nursing Diagnoses (5th cd). Upper Saddle River, NJ: Prentice I-Iall l-le.'llth, 2000;391.
Clucocorlicoids
Glucocorticoids can be evaluated by testing serum and urine cortisol
levels, 24-hour urinary corticosteroids, or ACTH. Altered glucocorticoid levels can affect protein and carbohydrate metabolism.
•
Serum cortisol levels are measured by RIA, which is indicated for
diagnosing Cushing's or Addison's disease. For accuracy, notation should
be made as to the time of day the serum was drawn, because levels are
