Pediatric Primary Care (137 page)

• Low energy.
• Significant loss of appetite.
f. May also present: explosive/destructive rages, separation anxiety, defiance of authority, bedwetting, night terrors, strong and frequent cravings, impaired judgment, impulsivity.
g. Presents with depressive symptoms and also exhibits ADHD-like symptoms that are very severe: Refer to mental health professional for further evaluation, particularly if family history of bipolar disorder.
D. Physical findings.
1. Specifically ask about thoughts of suicide or self-harm: suicide is third leading cause of death among 10-24-year olds.
2. Major depression may present with multiple, vague somatic complaints (e.g., headache, stomachache, fatigue, sleep, appetite changes).
3. Bipolar disorder may present with symptoms of ADHD, depression, mania, oppositional behavior.
E. Diagnostic tests.
1. Several screening tools useful for children/adolescents, including Children's Depression Inventory for ages 7-17 and Beck Depression Inventory for adolescents. Positive screens indicate need for comprehensive diagnostic evaluation by mental health professional.
2. Requires intensive interview with child/adolescent and family as well as detailed family history.
F. Differential diagnosis.
| Adjustment disorder, 309.9 | | Intermittent explosive disorder, 312.34 |
| Attention-deficit/hyperactivity disorder | | Oppositional defiant disorder, 313.81 |
| (ADHD), 314.01 | |
1. Adjustment disorder.
2. ADHD.
3. Intermittent explosive disorder.
4. Oppositional defiant disorder.
G. Treatment.
1. Major depression.
a. Antidepressant medication may be indicated.
• Consider SSRI medications:
i. Fluoxetine (Prozac): starting dose of 5 mg/day; increase to 15-40 mg/day for children, 10-60 mg/day for teens.
ii. Fluvoxamine (Luvox): starting dose of 25 mg/day; increase to 50-200 mg/day for children, 100-300 mg/day for teens.
iii. Sertraline (Zoloft): starting dose of 25 mg/day; increase to 50-150 mg/day for children, 50-200 mg/day for teens.
• Following remission of symptoms, continue medications
with
therapy for at least several months given high rate of relapse, recurrence of depression. Gradually discontinue medications over 6 weeks or longer.
b. Short-term psychotherapy such as cognitive behavioral therapy (CBT).
• CBT based on premise that young people with depression have distorted view of themselves, world, future. CBT focuses on changing distortions through time-limited therapy.
• Continued therapy for several months after remission of symptoms may help consolidate skills learned, cope with after effects of depression, address environmental stressors, understand how young person's thoughts and behaviors could contribute to relapse.
2. Bipolar disorder.
a. Use of mood-stabilizing medications such as lithium (Eskalith, Lithobid, lithium carbonate), valproic acid (Depakote), carbamazepine (Tegretol), lamotrigrine (Lamictal), tiagabine (Gabitril).
• Start lithium at 25 mg/kg/day, gradually increase until serum level reaches therapeutic range of 0.9-1.1 mEq/L.
• Valproic acid (Depakote): start at 15 mg/kg/day, gradually increase until serum level reaches therapeutic range of 80-120 mg/mL.
• Carbamazepine (Tegretol): starting dose of 100 mg/day with increase to 300-800 mg/day in children, 800-1000 mg/day in teens; monitor for serum level to reach therapeutic range of 8-12 mcg/mL.
b.Consider polypharmacy with addition of antipsychotic medications, calcium channel blockers, antianxiety agents.
c. Do not use antidepressant medication alone; may lead to mania or rapid cycling.
d. Psychostimulant medications frequently used to treat ADHD may worsen manic symptoms.
e. CBT, interpersonal therapy, multifamily support groups essential part of overall treatment plan.
H. Follow up.
1. Monitor effectiveness of medications; address side effects, compliance issues.
2. Monitor closely for suicidal thoughts and/or behaviors.
Note:
FDA Black Box warning on use of SSRI antidepressants in children and teens.
3. Monitor blood levels to assess appropriate medication dosing.
4. Collaborate with family, mental health treatment provider, school personnel to assess success of treatment approaches.
I. Complications.
| Conduct disorder, 312.9 | | Risk for suicide, 300.9 |
| Poor psychosocial functioning, V71.02 | | Substance abuse, 995.5 |
1. Increased risk for suicidal behavior: attempts may rise, particularly among adolescent males, if depression accompanied by conduct disorder or substance abuse.
2. Increased risk for poor psychosocial functioning.
3. School truancy or poor academic performance.
4. Substance abuse.
J. Education.
1. Monitor effectiveness of medications.
2. Educate families on signs/symptoms of both depression and mania and signs/symptoms of suicidal ideation.
BIBLIOGRAPHY
American Psychiatric Association.
Diagnostic and statistical manual of mental disorders.
4th ed. Washington, DC: Author; 2000.
National Institute of Mental Health.
Brief notes on the mental health of children and adolescents.
Bethesda, MD: Author; 2002.
National Institute of Mental Health. NIH Publication No. 00-4744. Bethesda, MD: Author; 2002.
National Institute of Mental Health. NIH Publication No. 00-4778. Bethesda, MD: Author; 2002.
National Institute of Mental Health. NIH Publication No. 01-4901. Bethesda, MD: Author; 2002.
Scahill L. Child and adolescent psychiatric nursing. In NL Keltner, CE Bostrom, & T McGuinness, eds.
Psychiatric nursing.
6th ed. pp. 459-468. St. Louis: Mosby; 2011.
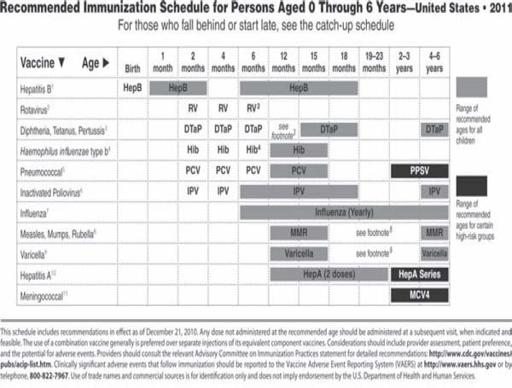
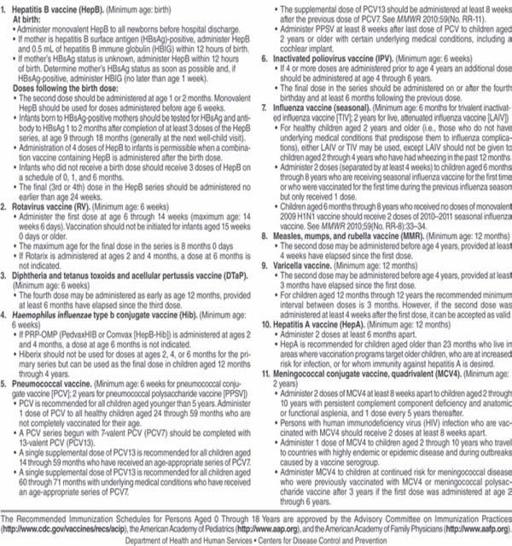
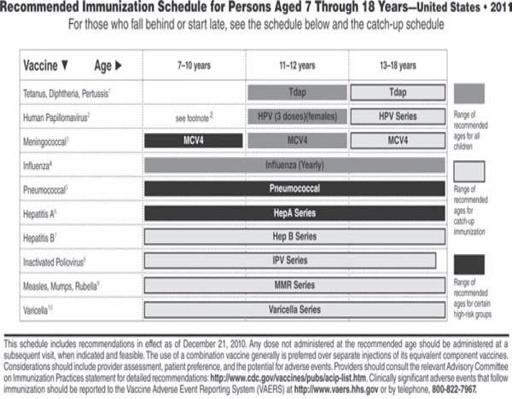
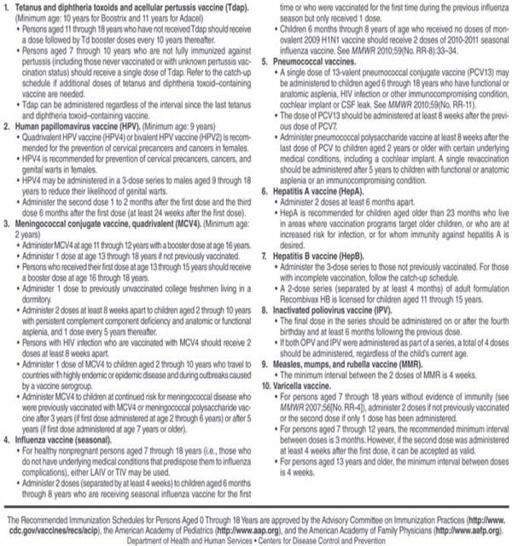
APPENDIX A
Recommended
Immunization Schedule
Other books
The Value of Vulnerability by Roberta Pearce
Murder in Ballyhasset by Noreen Mayer
The Unimaginable Mathematics of Borges' Library of Babel by William Goldbloom Bloch
Business Pleasures (Pleasures of the Heart) by Lia Davis
Claimed & Controlled: (Biker MC BBW Erotica) by Paige, Kirsten
The Keeper by Long, Elena
Sherlock Holmes: The American Years by Michael Kurland
My Reality by Rycroft, Melissa
The Story of Evil: Volume I - Heroes of the Siege by Tony Johnson
Chapel Noir by Carole Nelson Douglas