Pox (5 page)
Authors: Michael Willrich

Human beings appear to be universally susceptible to the variola virus. Unless they have been made immune by a previous infection with variola or another orthopoxvirusâsuch as cowpox or vaccinia, the principal viruses used in vaccinationâthey will almost certainly develop smallpox if the virus particles enter their respiratory tracts.
Together these facts about the variola virus begin to explain the epidemiology of smallpoxâits behavior in human communities. When the virus entered a population, smallpox tended to be passed around until most people had been infected. In small, relatively isolated populations, such as most towns of colonial North America, the virus would soon die out. The virus particles did not normally survive for long outside the human body, and when the ranks of vulnerable humans were exhausted, variola had no place to replicate. For smallpox to become
endemic
in a given population (prevalent for a long period at a relatively low level), there had to be a steady influx of susceptible bodies, whether through significant levels of in-migration or by natural reproduction. This is why in societies where endemic smallpox existed, such as European or English cities in the eighteenth century, small-pox was known as a disease of children. Most children born in London had smallpox before their seventh birthdays; the disease was a rite of passage. In English towns, nine out of ten fatal smallpox cases occurred in children under five. It was endemic smallpox that the nineteenth-century British historian Lord Thomas Macaulay famously called “the most terrible of all the ministers of death.” “The smallpox was always present,” he wrote, “filling the churchyard with corpses, tormenting with constant fear all whom it had not yet stricken, leaving on those whose lives it spared the hideous traces of its power, turning the babe into a changeling at which the mother shuddered, and making the eyes and cheeks of the betrothed maiden objects of horror to the lover.”
24
endemic
in a given population (prevalent for a long period at a relatively low level), there had to be a steady influx of susceptible bodies, whether through significant levels of in-migration or by natural reproduction. This is why in societies where endemic smallpox existed, such as European or English cities in the eighteenth century, small-pox was known as a disease of children. Most children born in London had smallpox before their seventh birthdays; the disease was a rite of passage. In English towns, nine out of ten fatal smallpox cases occurred in children under five. It was endemic smallpox that the nineteenth-century British historian Lord Thomas Macaulay famously called “the most terrible of all the ministers of death.” “The smallpox was always present,” he wrote, “filling the churchyard with corpses, tormenting with constant fear all whom it had not yet stricken, leaving on those whose lives it spared the hideous traces of its power, turning the babe into a changeling at which the mother shuddered, and making the eyes and cheeks of the betrothed maiden objects of horror to the lover.”
24
Of course, the “speckled monster” earned its worldwide infamy by its horrific epidemics. Major smallpox epidemics arose in two distinct epidemiological situations. In a so-called virgin soil population, one that had never been afflicted with smallpox or had been spared the virus for many years, a single epidemic could be devastating. In 1241, the people of Iceland had such an encounter with variola: some twenty thousand of the island's seventy thousand people died. The experience of indigenous populations of the Americas with epidemics of smallpox after the arrival of the Europeans in 1492 is well known if not easily fathomed. Many factors may have contributed to the extraordinarily high susceptibility of sixteenth-century American Indians to smallpox, including malnutrition, dislocation, and povertyâproblems caused or exacerbated by the violent process of European colonization. But the likelihood that American Indians and their ancestors had no previous contact with the disease helps explain mortality rates that ran from 50 to 80 percent. Variola was the deadliest killer in a terrible onslaught of alien microorganisms that, by some historical estimates, may have decimated as much as 90 percent of the precontact population of the Americas.
25
25
A different sort of epidemic occurred in well-populated places where smallpox was more or less always present, such as parts of late eighteenth-century Europe and England. The number of susceptible individuals in a community gradually built up over time, creating fodder for an “epidemic year,” when smallpox became suddenly widespread and lethal. In this situation, where a majority of the adult population, including most of the breadwinners, was immune from previous infection, an epidemic could cause untold misery without seriously threatening the population's subsistence.
26
26
As with many infectious diseases, the incidence of smallpox rose and fell with the seasons. Climate, social factors, and the traits of the virus itself conspired to make smallpox a disease of the winter and spring. Variola remained viable longer at cooler temperatures. And the tendency of humans to crowd together indoors during the winter months made the virus's journey from person to person a short one.
Turn-of-the-century medical experts, well versed in the germ theory, assumed that some life form, invisible to the naked eye, caused smallpox. But they could only guess at its nature. “The contagious principle, probably a microbe, has not been discovered,” declared an authoritative 1899 pamphlet, prepared by Marine-Hospital Service scientists for Surgeon General Wyman. Since the introduction of the germ theory, European and American scientists had hunted for the disease agent under their microscopes. A few reported seeing traces of smallpox “germs.” Orthopoxviruses are among the largest known viruses, but they are still extremely small. According to one modern writer, it would take three million of them, laid out in rows, to pave over a standard typographic period. An actual sighting would not be possible until the invention of the electron microscope in the 1930s. In 1947 Canadian and American scientists finally viewed the particles, or virions, of variola.
27
27
Since that time, variola virions have often been called bricks, because of their shape: a three-dimensional rectangle with slightly rounded edges. The name fits for other reasons as well. Each virion is made up of a combination of a hundred different proteins, which interlock in a structure so durable that it enables the virions to survive for a time in the open air. The knobby protein exterior of each brick protects the genetic jewel within: a molecule of double-stranded DNA. By attaching itself to and then penetrating a susceptible cell, usually in the mucous membranes of the throat or lungs, a single virion has the power to trigger an unstoppable process of genetic replication that can turn a healthy person into a corpse.
28
28
For all of its mysteries, the clinical features of smallpox were fairly well understood in January 1899, when Surgeon General Wyman issued his “Précis upon the Diagnosis and Treatment of Smallpox.” The timing was significant. The disease was invading communities, mostly in the South, where neither the laypeople nor the physicians had seen a bona fide case of smallpox in many years, if ever. The “Précis” was, in no small measure, a political document. Wyman aimed to remind people of the necessity of vaccination, to shore up confidence in the nation's vaccine supply, to clarify the national government's limited responsibilities, and to spur the fiscally conservative local and state governments to take action.
29
29
Wyman's officers in the Marine-Hospital Service disseminated the “Précis” widely, especially in the South. The report reflected state-of-the-art American medical knowledge about smallpox. Wyman's description of the clinical course of smallpox squares with descriptions of the disease found in medical treatises and journals from the period, as well as the accounts of local cases written by physicians such as Dr. Henry Long. The vast scientific literature on smallpox produced since that time has generally confirmed that clinical picture, while shedding new light on the virological and pathological processes that underlay the disease. Unlike the vast majority of physicians alive today, these turn-of-the-century experts had firsthand experience with smallpox. For them smallpox was not a frozen stockpile preserved, like ancient DNA sealed in amber, in a carefully guarded government laboratory vault and read about in medical journals. For them small-pox was still a part of the known world.
30
30
Perhaps the most significant misunderstanding about smallpox shared by the authors of the “Précis” and many of their scientific contemporaries had to do with the mechanics of disease transmission. They understood correctly that smallpox could be spread by the passage of “the microbe” from one person's respiratory system to another's. In fact, a person suffering from smallpox shed virions in each droplet of saliva. A single breath, cough, laugh, sigh, or spoken word was enough to launch the virions into the air. When one or more particles touched down upon the mucous membrane of another person's mouth, nose, throat, or lungs, the process of viral replication began within hours.
Where the “Précis” went wrong was in its insistence that such face-to-face contacts constituted a lesser threat than did the scabs and crusts of dried pus that fell from the skin of a convalescent patient. “The contagion is tenacious,” the “Précis” stated, “and may be conveyed by persons and by fomites, such as hair, clothing, paper, letters, furniture, etc., or it may be spread through the air by means of the wind blowing the dust containing the virus.” This belief in the infectious power of “fomites,” contaminated objects of countless variety, led to the conclusion that smallpox was what nineteenth-century sanitarians called a “filth disease”âdangerous to all but spread chiefly by the lower orders. As the “Précis” put it, smallpox was “more common among the colored races, probably on account of their condition of living in small, crowded rooms, with slight regard for cleanliness.”
31
31
The “Précis” got the infective nature of variola about half-right. The crowded sleeping quarters that the world's poorest people called homeâbe it a sharecropping family's one-room cabin or a bamboo hutâwere prime variola territory. It surprised no one when, two weeks after Harvey Perkins shared a hut with two other workers at Neal's Camp, reports reached Charlotte that two cases of smallpox had broken out in the encampment. There were obvious obstacles to maintaining personal hygiene and health under such circumstances. Still, scientists now believe that “filth” had little to do with the spread of smallpox. Laboratory tests have shown that the virions in smallpox scabs can, under optimal conditions, retain their infectivity for years. But the virions are so tightly bound within the hard fibrin mesh of the scab that it takes heavy grinding to release them. For this reason, many experts have concluded that fomites were “relatively unimportant” transmitters of infection, compared with the spread of virions in sneezes and coughs. This does not mean that infection by fomites never occurredâcontaminated bed linen, in particular, readily transmitted infectionâbut the long-standing association of smallpox with the filthy poor was grounded more in class and racial bias than in medical reality.
32
32
Â
Â
O
nce the first virion penetrated the first cell in a person's respiratory tract, the incubation period began. During this period, most people presented no symptomsâperhaps a little malaise or gastric discomfort. Meanwhile, the variola bricks silently but explosively replicated and spread in the host's lymph nodes, spleen, and bone marrow. Over time, the virions piling up in the patient's cells would number in the quadrillions. The incubation normally lasted from ten to fourteen days. The “Précis” gave twelve days as the norm. Such medical facts determined the politics of smallpox control. Conservative health officials enforced two weeks as the term a smallpox “suspect,” showing no symptoms, could be held against her will in a quarantined house or detention camp.
33
nce the first virion penetrated the first cell in a person's respiratory tract, the incubation period began. During this period, most people presented no symptomsâperhaps a little malaise or gastric discomfort. Meanwhile, the variola bricks silently but explosively replicated and spread in the host's lymph nodes, spleen, and bone marrow. Over time, the virions piling up in the patient's cells would number in the quadrillions. The incubation normally lasted from ten to fourteen days. The “Précis” gave twelve days as the norm. Such medical facts determined the politics of smallpox control. Conservative health officials enforced two weeks as the term a smallpox “suspect,” showing no symptoms, could be held against her will in a quarantined house or detention camp.
33
When the symptoms finally came, they struck with such unexpected force that the “Précis” called the onset the “Invasion.” The patient felt a sudden chill, followed by severe pain in the loins and lower back, a splitting headache, and a high fever, in some cases surging to 106 degrees F. The pulse raced. Many patients vomited. The tongue grew thick with a brown coating; the appetite vanished, but the thirst was unquenchable. Some adults grew delirious. Some children were rocked by convulsions.
34
34
In this early phase, as Dr. Long learned while attending to patients in the Iredell County pesthouse, smallpox remained inscrutable even to the trained medical eye. It could be typhoid fever, malaria, la grippe, or dengue. For the patient, these feverish days felt like a bad case of the flu, and some managed to carry on with their work. President Abraham Lincoln is believed to have been fighting the preeruptive fever of smallpox when he delivered the Gettysburg Address on November 19, 1863. One listener described the president's appearance as “sad, mournful, almost haggard.” The rash appeared two days later.
35
35
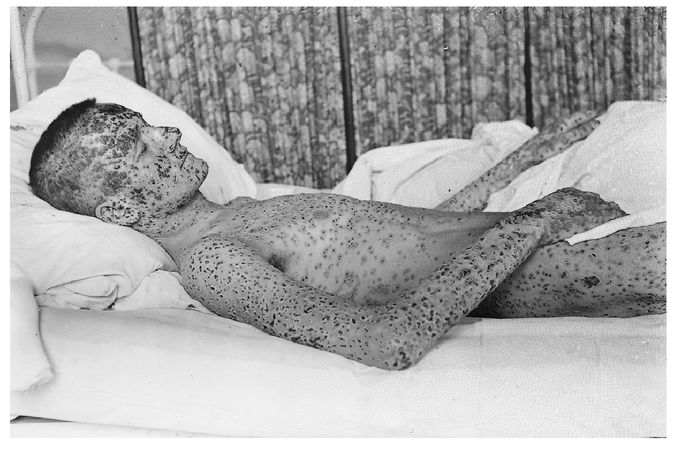
Smallpox patient from the Cleveland epidemic of 1901â03. This photograph was taken by Dr. Homer J. Hartzell, who headed the city's smallpox hospital.
COURTESY OF THE DITTRICK MEDICAL HISTORY CENTER, CASE WESTERN RESERVE UNIVERSITY
COURTESY OF THE DITTRICK MEDICAL HISTORY CENTER, CASE WESTERN RESERVE UNIVERSITY
Â
In a typical case, the fever fell by the second or third day. The constitutional symptoms abated. The patient felt better. So much so, a nineteenth-century nurse's manual noted, that he might “suppose himself convalescent.” Unknown to the patient, the lesions had already begun rising, about twenty-four hours earlier, on the mucous surfaces of the mouth, the back of the throat, and more generally throughout the alimentary and respiratory tracts. Modern virologists call this eruption the “enanthem.” The enanthem turned the patient into a veritable mist machine of infection. The lesions evolved rapidly and broke down within two or three days, releasing virions in vast quantities into the saliva. For the next week or more, the patient's every breath might launch a fusillade of invisible infective particles into the air. Although the patient could remain infectious for weeks, twentieth-century studies concluded that smallpox sufferers were most likely to infect others during the first week of their skin rash.
36
36
Other books
Chicken Soup for the Woman's Soul by Jack Canfield
Musicophilia: Tales of Music and the Brain by Oliver W. Sacks
Eugénie: The Empress & her Empire by Seward, Desmond
Skin by Patricia Rosemoor
Illicit Desire: Outlawed Realm, Book 2 by Tina Donahua
Gregory, Lisa by Bonds of Love
Elemental by Emily White
Tete-a-Tete by Hazel Rowley
Josh's Justice, Cowboy Romance (Bad in Boots, Book 4) by Michelle, Patrice
The Well of Wyrding (Revenant Wyrd Book 3) by Travis Simmons