Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (1102 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

Rapid intraoperative PTH that declines ≥50% from the highest baseline in 10 minutes after resection indicates successful total excision.
PARATHYROID HORMONE–RELATED PEPTIDE (PTHrP)
Definition
PTHrP is a protein secreted by some cancer cells leading to humoral hypercalcemia of malignancy (HHM). It shares the same 13 N-terminal amino acids as PTH; however, the remaining structure is different. PTHrP is larger than PTH and contains 139–173 amino acids compared to 84 for PTH. PTHrP shares many actions with PTH leading to increased calcium release from bone, reduced renal calcium excretion, and reduced renal phosphate reabsorption. However, PTHrP does not produce the normal anion gap metabolic acidosis commonly found with hyperparathyroidism. See Tables 16.61–16.63 and Figures 16.2 and 16.3.
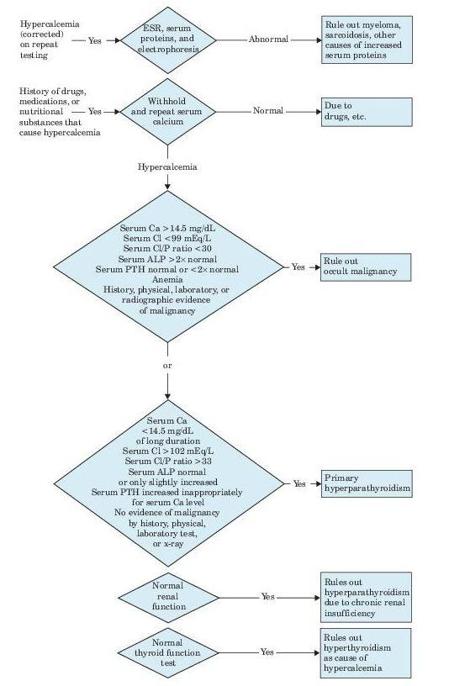
Figure 16–2
Algorithm for diagnosis of hypercalcemia. (ESR, erythrocyte sedimentation rate; PTH, parathyroid hormone.) (Data from Wong ET, Freier EF. The differential diagnosis of hypercalcemia: an algorithm for more effective use of laboratory tests.
JAMA.
1982;247:75 and Johnson KR, Howarth AT. Differential laboratory diagnosis of hypercalcemia.
CRC Crit Rev Clin La Sci.
1984;21:51.)
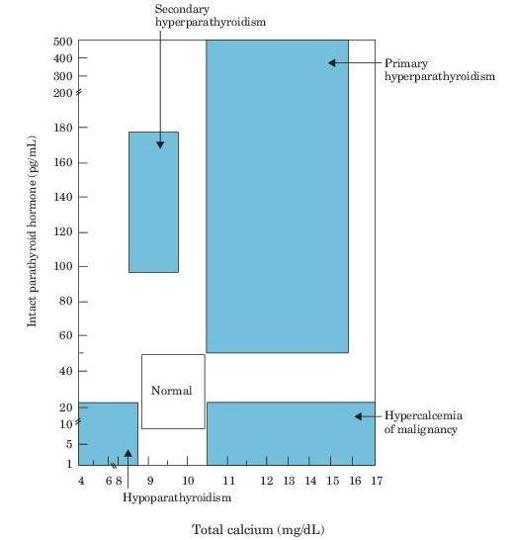
Figure 16–3
Diagrammatic illustration of distribution of patients according to serum calcium and serum PTH. The values of some patients may lie outside the exact boundaries indicated, and some conditions may overlap. The exact cutoff will vary somewhat with the assays used, the patient mix, and the locally established normal reference ranges. (From
Mayo Laboratories Test Catalog
. Rochester, MN: Mayo Medical Laboratories; 1995. By permission of Mayo Foundation for Medical Education and Research. All rights reserved.)
TABLE 16–61. Serum Calcium and PTH in Various Conditions
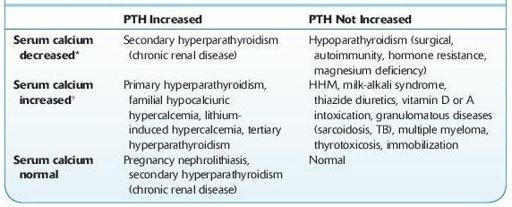
HHM, humoral hypercalcemia of malignancy; PTH, parathyroid hormone.
*PTH may be normal or increased in hypocalcemic patients due to renal failure, acute pancreatitis, vitamin D deficiency.
†
PTH may be normal or increased in hypercalcemic patients due to acromegaly, vitamin A intoxication, MEN type
IIA, RTA, chronic renal failure.
TABLE 16–62. Laboratory Findings in Various Diseases of Calcium and Phosphorus Metabolism
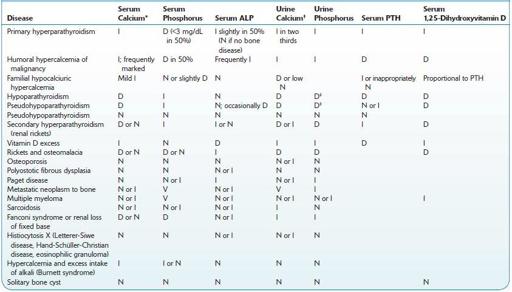
D, decreased; I, increased; N, normal; V, variable.
*Serum calcium. Repeated determinations may be required to demonstrate abnormalities. Serum total protein level should always be known. See also response to cortisone.
†
Urine calcium. The patient should be on a low-calcium diet (e.g., Bauer-Aub).
‡
See Ellsworth-Howard test.
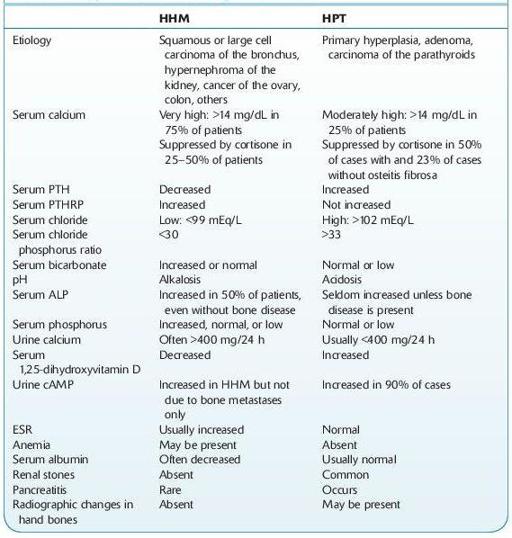
TABLE 16–63. Comparison of Primary Hyperparathyroidism (HPT) and Humoral Hypercalcemia of Malignancy (HHM)
Use
PTHrP is useful clinically in differentiating primary hyperthyroidism from HHM. Also useful as a marker in the management of patients with tumorassociated hypercalcemia.
The usual pattern of HHM is elevated total and ionized calcium, low PTH in the absence of other causes of hypercalcemia (e.g., excessive vitamin D, sarcoid, TB). If the presence of a malignancy is uncertain, or there are several possible causes for hypercalcemia, measurement of PTHrP can be of assistance.