Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (21 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

BOOK: Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis
4.02Mb size Format: txt, pdf, ePub
Thrombocytopenia, neutropenia, or lymphopenia are usually immune in origin.
Serum complement C3 and C4 levels are decreased in parallel with disease activity.
ESR and CRP are often elevated in active disease.
Renal function studies are indicated to assess renal involvement.
Presence of cryoglobulins may correlate with disease activity.
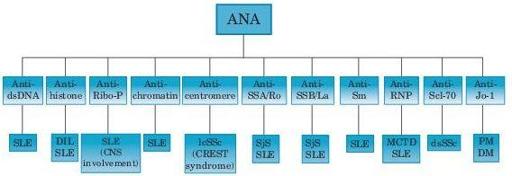
Figure 2–1
Role of antinuclear antibodies in the diagnosis of connective tissue diseases. ANA, antinuclear antibodies; CNS, central nervous system; DIL, drug-induced lupus erythematosus; DM, dermatomyositis; dsDNA, double-stranded DNA; dsSSc, diffuse cutaneous scleroderma; lcSSc, limited cutaneous scleroderma; MCTD, mixed connective tissue disease; PM, Polymyositis; Ribo-P: ribosomal P protein; RNP, U1 ribonucleoprotein; SjS, Sjögren syndrome; SLE, systemic lupus erythematosus; Sm, Smith.
Suggested Reading
Rahman A, Isenberg DA. Systemic lupus erythematosus.
N Engl J Med.
2008;358:929–939.
SYSTEMIC SCLEROSIS (SCLERODERMA)
Definition
Systemic sclerosis (SSc) is a complex, progressive disease characterized by extensive fibrosis, vascular alterations, and multiple system involvement.
SSc is subcategorized into two distinct subtypes, depending on the extent of skin involvement:
Limited cutaneous scleroderma (lcSSc): fibrosis is mainly restricted to the hands, arms, and face. Patients typically display features of the CREST syndrome (calcinosis, Raynaud phenomenon, esophageal motility dysfunction, sclerodactyly, and telangiectasia).
Diffuse cutaneous scleroderma (dsSSc): rapidly progressive and affects large areas of the skin and one or more internal organs. Sclerosis skin is found on the chest, abdomen, or upper arms or shoulders.
Patients with scleroderma plus evidence of SLE, rheumatoid arthritis, polymyositis, or Sjögren syndrome are considered to have overlap syndrome.
Other books
SERIAL UNCUT by J.A. Konrath, Jack Kilborn, Blake Crouch
Murder by Chance (Betty Chance Mystery) by Dennis, Pat
Perfectly Flawed by Nessa Morgan
A Madness in Spring by Kate Noble
Huntress by Trina M Lee
Twice Driven by Madison Faye
Vanguard (Ark Royal Book 7) by Christopher Nuttall
The Strange Maid by Tessa Gratton