Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (559 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

BOOK: Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis
11.53Mb size Format: txt, pdf, ePub
This condition, which involves amyloid deposition in the kidneys, is one of the most frequent complications of AA, AL, and several hereditary forms of amyloidosis.
Who Should Be Suspected?
Candidates include patients with known systemic amyloidosis who develop proteinuria or, in the absence of this diagnosis, individuals with new-onset proteinuria, renal insufficiency, or nephrotic syndrome of unknown etiology.
Laboratory Findings
Urinalysis: persistent proteinuria, associated with glomerular deposits of amyloid. Proteinuria varies from mild, with or without hematuria, to massive with urinary protein excretion rate in the nephrotic range (>3.5 g/day) and may exceed 20 g/day. Urinary protein is mostly albumin. Urine sediment is typically benign.
GFR is reduced, and serum creatinine concentration is moderately elevated.
Hypoalbuminemia and other findings secondary to the nephrotic syndrome are seen in advanced cases. ESRD develops in 20% of renal amyloidosis patients with nephrotic syndrome.
Nephrogenic diabetes insipidus (DI) and renal tubular acidosis may result from tubular deposition of amyloid.
Suggested Reading
Dember LM. Amyloidosis-associated kidney disease.
J Am Soc Nephrol.
2006;17:3458–3471.
DIABETIC NEPHROPATHY
Overview
See diabetes mellitus (DM).
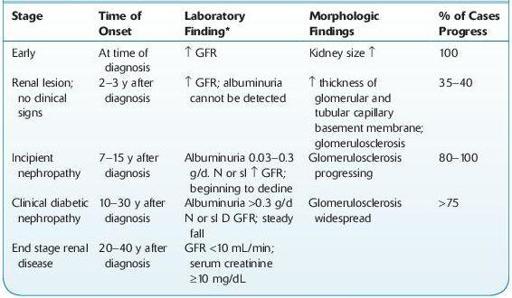
Diabetic nephropathy (DN), also referred to as diabetic kidney disease or Kimmelstiel-Wilson disease, is characterized by persistent proteinuria and progressive renal insufficiency in diabetic patients in the absence of other renal diseases. Approximately one third of patients with diabetes develop DN years after diagnosis. DN is the most common cause of ESRD in the United States and Europe, with ESRD incidence of 30% in type 1 DM and up to 20% in type 2 DM (see Table
12-7
).
Microalbuminuria is an early sign of the development of DN and has very high specificity and positive predictive value for subsequent DN. It is also associated with a longer duration of diabetes, poorer glycemic control, higher blood pressure, development of more advanced retinopathy and neuropathy, subsequent renal failure, increased vascular damage, and risk for cardiovascular disease.
TABLE 12–7. Evolution of Renal Disease in Insulin-Dependent Diabetes Mellitus (IDDM)
Other books
The Beckoning Lady by Margery Allingham
At Wick's End (Book 1 in the Candlemaking Mysteries) by Tim Myers
The Courage Consort by Michel Faber
Knight Triumphant by Heather Graham
Stacey And The Mystery Of Stoneybrook by Ann M, Martin
Nowhere to Run by C. J. Box
TIMBER: The Bad Boy's Baby by Frankie Love
Lure of the Wicked by Cooper, Karina
All This Time by Marie Wathen
Queermance Anthology, Volume 1 by Lindy Cameron