Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (65 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

BOOK: Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis
9.94Mb size Format: txt, pdf, ePub
Definition
Hyperlipidemia is an elevation of lipids (cholesterol, cholesterol esters, phospholipids, and triglycerides) in the bloodstream; is a risk factor for coronary heart disease (CHD); and promotes atherosclerosis. Lipids are transported as lipoproteins in the body; there are five major types: chylomicrons, VLDLs, intermediate-density lipoproteins (IDLs), LDLs, and HDLs. The protein portions of the lipoprotein are referred as apolipoprotein, of which there are six major classes (A, B, C, D, E, and H) and numerous subclasses (AI, AII, AIV, AV, B48, B200, CI, CII, CIII, and CIV).
The diagnosis of primary hyperlipidemia is made after the secondary causes are evaluated and ruled out or attempt is made to treat or eliminate the underlying cause. Secondary causes of dyslipidemia and associated lipid changes include some underlying disease, organ failure, or some drugs. It is not uncommon to have some overlap, with dyslipidemia being attributed to both primary and secondary causes (Table
3-2
).
Historically, primary dyslipidemias, such as the familial dyslipidemias, have been grouped according to the electrophoretic activity. The primary dyslipidemias are associated with overproduction and/or impaired removal of lipoproteins. A potentially more useful presentation of primary lipidemias is to classify them according to the principal lipid abnormality (Table
3-3
).
TABLE 3–2 Diseases That May Cause Dyslipidemia and Associated Lipid Changes
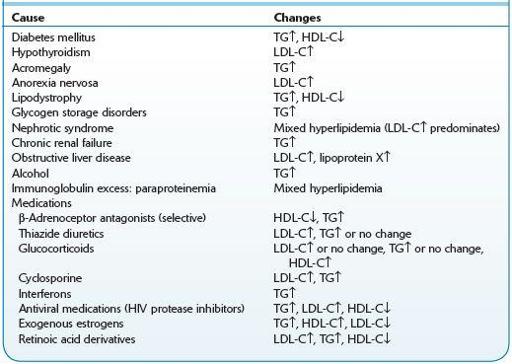
HDL-C, high-density lipoprotein–cholesterol; LDL-C, low-density lipoprotein–cholesterol; TG, triglyceride; ↑, increased levels; ↓, decreased levels.
TABLE 3–3 Classificationof Familial Dyslipidemias According to Predominant Lipid Abnormality and Etiology
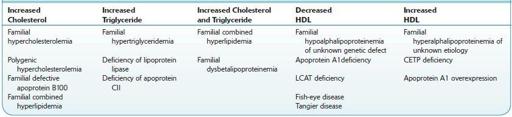
CETP,cholesterylestertransportprotein;HDL,high-densitylipoprotein;LCAT,lecithin–cholesterolacyltransferase;TG,triglyceride.
Who Should Be Suspected?
There are typically no symptoms associated with hyperlipidemia, and it tends to be discovered during routine examination or evaluation for atherosclerotic cardiovascular disease. Detection of cholesterol disorders and other CHD risk factors occurs primarily through clinical case findings. On occasion, symptoms can include xanthomas around the eyes, Achilles tendons, and the extensor tendons of the hands, particularly with familial forms of the disorder.
Individuals with higher lipid levels may develop lipemia retinalis (white appearance of the retina), arcus senilis (white discoloration of the peripheral cornea), or pancreatitis.
Laboratory Findings
Core laboratory: Standard lipid profile—total cholesterol (TC), LDL cholesterol, HDL cholesterol, and triglycerides (TGs)—should be obtained at least once every 5 years in adults age 20 and older.
Low-risk persons: Further testing is not required if the HDL-cholesterol level is ≥40 mg/dL and TC is <200 mg/dL.
Other books
Titan (GAIA) by Varley, John
Equal Access by A. E. Branson
The Second Spy: The Books of Elsewhere: Volume 3 by West, Jacqueline
Death in a Funhouse Mirror by Kate Flora
Ransom Game by Howard Engel
Why We Buy by Paco Underhill
Gingham Mountain by Mary Connealy
Twisted Desire by Laura Dunaway
The House Above the River by Josephine Bell
Framed by C.P. Smith