Water: For Health, For Healing, For Life (11 page)

I recommend to asthmatics who are about to get an attack, or are in the middle of an asthma attack, to drink two or three glasses of water, and then put a pinch of salt on their tongue. Water and salt will tell the brain that the missing components in a dehydrated body—in asthmatics in particular—have entered the system. The brain will immediately instruct the bronchioles to relax, and breathing will become much easier. When the salt reaches the lungs, salt pumps secrete it in the bronchioles to loosen the mucus plugs and prepare them to be carried away—
only when water is available.
Too much salt and
not enough water
may do the opposite. It might cause constriction of the bronchioles.
This is why phlegm always tastes salty. Salt is essential to keep the airways of the body clear—including the nasal passageways when you have a cold. Salt also unplugs mucus in the nose and the sinuses and stops runny nose in allergic reactions.
BLOOD PRESSURE AND DEHYDRATION
The measurable force that rushes blood through the arterial system of the body is called blood pressure. This force has two components. The diastolic component is the constant basic force in the arteries that keeps the blood vessels full and under a constant basic pressure. It is the lowest reading on the measuring instruments. The normally accepted figure for this reading is between 60 and 90. The systolic component of blood pressure is the sharp rise in force inside the arteries, produced by the contraction of the left side of the heart when it forces the volume of blood in its ventricle into an already filled and under-pressure arterial system. The normal range is between 90 and 130. In other words, the accepted normal blood pressure—systolic over diastolic—is from 90 over 60 to 130 over 90.
The difference in the two readings is significant. It means that the blood is being stirred by the rush of new blood in the arteries, which prevents blood's heavier constituents from sedimenting in the stagnant areas; it means an added pressure that will squirt some clear serum through the tiny holes in the capillaries and into the filtration areas in the kidneys for cleansing of the blood. The significance of the diastolic pressure is in its effect of filling all the blood vessels of the body so none remains empty.
The problem of blood circulation becomes apparent if the diastolic pressure rises well above or falls well below the normal range. If it rises above the range, it means the heart has much more pressure to work against when forcing blood into the circulation. For a short period of time, it is not a big deal. But given sixty to eighty beats a minute, day in and day out, you will have one very tired heart, as well as over-shocked blood vessels that have to become thick and inelastic to withstand the repeated onslaught. Diastolic pressure well below normal affects circulation, especially to the brain. Not enough pressure in the arteries that go to the brain means less oxygen reaching the vital brain centers. The result: feeling faint and not fully focused. With low blood pressure, you can actually faint if you stand up suddenly. How do these complications arise?
Dehydration!
High Blood Pressure
Roughly sixty million Americans suffer from hyper-tension or high blood pressure. There may be more than one reason when blood pressure readings register an increase from what is considered normal. In my scientific opinion, the most common and frequent reason is a gradually establishing dehydration in the body. This type of hypertension is labeled “essential hypertension.” A large number of people in this group receive some form of medication to deal with this dehydration signal of the body. Until they learn about the relationship of this condition to their insufficient water intake, or a wrong choice of fluid intake, they will have to continue taking pharmaceutical products for the rest of their shortened lives.
The paradigm shift offers us a new perspective on high blood pressure—the form we call essential hypertension. It tells us that a gradual rise in blood pressure is an indicator of a gradually establishing shortage of water in the body. The blood vessels of the body have been designed to cope with repeated fluctuations in their blood volume and the circulation requirements of the tissues they supply. They have tiny holes or lumen that open and close to adapt to the amount of blood inside them. In water loss from the body— rather, lack of sufficient water intake—66 percent of the deficit is reflected in the volume of water held in some cells of the body (plumlike cells begin to become prunelike); 26 percent is reflected in the fluid environment outside the cells; and only 8 percent of the deficit is imposed on the volume held in blood circulation. The circulatory system adapts to its 8 percent loss by shrinking in capacity. Initially, peripheral capillaries close down, and eventually the larger vessels tighten their walls to keep the blood vessels full.

Figure 7.1:
The vascular system all over the body adapts to blood volume loss by selective closing of the lumen. One major cause for blood volume loss is the loss of body water or its undersupply through the loss of thirst sensation.
This tightening leads to a measurable rise in tension in the arteries. This is called hypertension. If the blood vessels did not tighten on the void, gases would separate from the blood and fill the space, causing gas locks. This vascular adaptation to the amount of water the vascular system carries is a most advanced design within the principle of hydraulics that the blood circulation of the body is modeled on.
Injection Pressure for the Filter Systems
Another major reason for the tightening of the vessels is the need to squeeze the blood volume in the arterial system so that water can be filtered and injected into some vitally important cells in the body, such as the brain cells. The tightening of the blood vessel walls provides the force necessary to operate a reverse osmosis system in the human body—a crisis-management program to keep important cells alive. Water is pushed into selected cells of the body through tiny “shower-heads”—cluster perforations in the cell membrane. The difference between the two readings of blood pressure is the range of force needed to deliver water under normal circumstances into some vital cells of the body. As the body becomes more and more dehydrated, the amount of pressure needed to filter and inject water into vital cells increases. The less water there is in the body, the more pressure is needed to hydrate vital cells.
The mechanism is simple. When confronting stressful circumstances, and in dehydration that is becoming gradually established, histamine is released. Histamine activates the production of vasopressin (an antidiuretic hormone). Certain cells of the body have receiving points that are sensitive to vasopressin. As soon as the hormone sits on the sensitive point, a hollow showerhead type of opening with minute holes in its base is created in the cell membrane. Serum fills the space, and its water content filters through the holes, which are large enough for the passage of only one water molecule at a time. Vasopressin, as its name implies, also produces the tightening of the vessels around it. This tightening of vessels translates into a squeeze that pushes the serum and its water through the holes in the blood vessel—a necessary act if some of this water is to be pushed back into the cells.
Renin-Angiotensin System
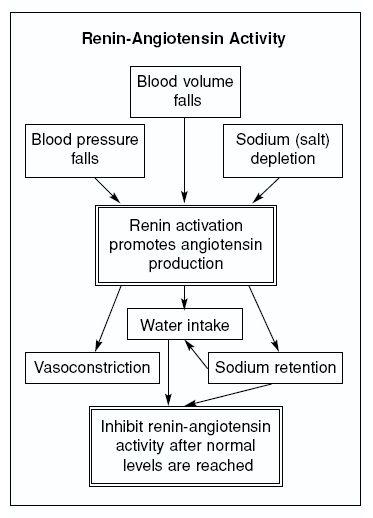
Another water-regulatory system that is associated with dehydration and histamine production is the brain's renin-angiotensin (RA) system. RA production is a component of the thirst sensation and increased water intake. It also produces some tightening of the blood vessels and has been recognized as a dominant factor in the production of hypertension. The RA system eventually becomes prominent in the kidneys, which have to concentrate urine and save water while producing urine. The kidneys recognize water shortage and activate their resident RA system so that more water is called in for urine production. The RA system eventually stimulates a drive for salt intake and its retention until the body is fully hydrated. The brain has an independent RA system of its own. When there is a water shortage, the centers that sense this shortage become active and produce the neurotransmitter histamine, which will then activate the brain's RA system.
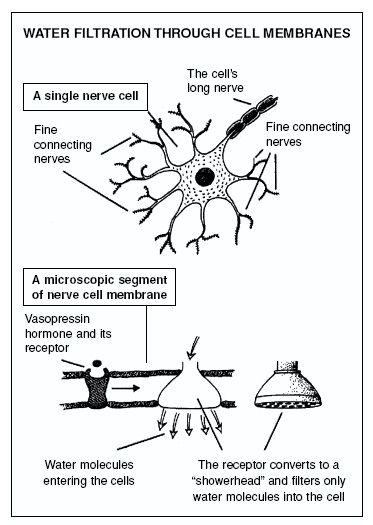
Figure 7.2:
The schematic model of a nerve cell, its membrane wall, and the vasopressin receptor that becomes transformed into a type of “showerhead” that lets only water through its very small perforations. This is part of the mechanism of reverse osmosis that the body employs to deliver filtered water into vital cells.
There is a simultaneous rise in blood pressure when the body is dehydrated inside its cells. The tendency is to begin to retain salt, which is essential for the operation of the reverse osmosis process. The body collects water in the form of edema fluid, from which free water is filtered and then injected into vital cells. We in medicine have not recognized the relationship of dehydration inside the cells of the body to the physiological role of RA system. We have only recognized the expansion of water volume in the environment outside the cells. We automatically assume that the retention of fluid in the body, and the rise in blood pressure, are pathological processes caused by the RA system. We have not realized that the process is an adaptive measure to correct dehydration inside the vital cells of the body, such as the brain cells, the liver cells, the kidney cells, the lungs, and other important organs and glands.
The chemical steps involve angiotensin-converting enzymes (ACE). In three steps, these enzymes produce
angiotensin III.
This chemical forces a strict drive for retention of salt in the body. Extra salt will retain extra water in the tissues.
The only things that turn off this salt-retaining-drive mechanism are adequate water intake and some salt intake that balance the fluid content inside and outside the cells. The salt should be unrefined sea salt that contains other vital minerals that are needed to hold on to the water once it is injected or diffused inside the cells.
When it is freely available, water diffuses quite rapidly through the cell membranes without needing to be forced. Its rate of diffusion through the cell membrane has been calculated to be 10
−3
centimeters per second, which is fairly fast. This natural and fast diffusion process of water in the kidneys is the reason why water itself is a natural diuretic—far better than chemical diuretics or ACE inhibitors now used routinely. In fact, to give a person with essential hypertension diuretics is, in my opinion, a blatant disservice to the patient.
Water itself will increase urine production, and excess retained salt will gradually be passed in the urine. This is why water is a most effective decongestant and edema remover. When you drink water to dilute the blood, it will not be necessary to rely entirely on the process of reverse osmosis and the RA system to force water into vital cells—including the renal tissue that has to make concentrated urine and force the toxic waste out of the body. The body will not cause a collection of extra fluid in the tissues as a reservoir to filter and inject water into its vital cells as an emergency process. This is what essential hypertension is all about.
Because it is associated with aging, and seemed unavoidable in the past, the gradual rise in blood pressure has been labeled “essential hypertension,” meaning it is an unavoidable outcome of living to a mature life. It was not recognized that a gradual loss of thirst perception as we grow older is responsible for the onset of chronic dehydration and subsequent hypertension.