What to expect when you're expecting (205 page)
Read What to expect when you're expecting Online
Authors: Heidi Murkoff,Sharon Mazel
Tags: #Health & Fitness, #Postnatal care, #General, #Family & Relationships, #Pregnancy & Childbirth, #Pregnancy, #Childbirth, #Prenatal care

Once you know the cause, or causes, you can talk to your practitioner about treatment options, as well as how best to care for the next pregnancy. Surgery may correct some uterine and cervical issues; thyroid medication can easily treat a thyroid condition, and medically supervised supplementation can just as easily resolve a vitamin deficiency; hormone treatments may also help, as can tests for antibodies and treatment to prevent blood clots (low-dose aspirin and/or heparin). In some instances, patients with a history of early miscarriages who appear to be producing too little progesterone may benefit from taking the hormone, though this treatment is controversial. Or, if excess prolactin is the cause, medication to reduce prolactin levels in the mother’s blood may allow a pregnancy to proceed to term.
Even if you’ve had repeated miscarriages, you still have a good chance of sustaining a successful pregnancy in the future. But that may be hard for you to believe or even to hope for. It will be important to find ways of managing your understandable fear that becoming pregnant again will mean you’ll miscarry again. Yoga, visualization techniques, and deep-breathing exercises can help with the anxiety, and support can come from other women who’ve suffered similar losses. Sharing your feelings openly with your partner may also help. Remember, you’re in this together.
If you’re experiencing the type of heavy bleeding and painful cramping that signal a miscarriage, there’s usually nothing, unfortunately, that can be done to stop the inevitable. The further along your pregnancy, the more likely your practitioner might bring you into the hospital. Performing a D and C may be necessary to remove any remnants of the pregnancy.
Can it be prevented?
Once a late miscarriage is under way, it isn’t preventable. But if the cause of a late miscarriage can be determined, it may be possible to prevent a repeat of the tragedy. If a previously undiagnosed incompetent cervix was responsible, future miscarriages can be prevented by cerclage early in pregnancy, before the cervix begins to dilate. If chronic disease, such as diabetes, hypertension, or a thyroid condition, is responsible, the condition can be brought under control prior to any future pregnancy. Acute infection can be prevented or treated. And an abnormally shaped uterus or one that is distorted by the growth of fibroids or other benign tumors in some instances can be corrected by surgery. The presence of antibodies that trigger placental inflammation and/or clotting may be treated with low-dose aspirin and heparin injections in a subsequent pregnancy.
What is it?
An ectopic pregnancy (also known as a tubal pregnancy) is one that implants outside the uterus, most commonly in a fallopian tube, usually because something (such as scarring in the fallopian tube) obstructs or slows the movement of the fertilized egg into the uterus. An ectopic pregnancy can also occur in the cervix, on the ovary, or in the abdomen. Unfortunately, there is no way for an ectopic pregnancy to continue normally.
Ultrasound can detect an ectopic pregnancy, often as early as five weeks. But without early diagnosis and treatment of an ectopic pregnancy, the fertilized egg might continue to grow in the fallopian tube, leading to a rupture of the tube. If the tube bursts, its ability in the future to carry a fertilized egg to the uterus is destroyed, and if the rupture is not cared for, it can result in severe, even life-threatening, internal bleeding and shock. Luckily, quick treatment (usually surgery or medication) can help avoid such a rupture and removes most of the risk for the mother while greatly improving the chances of preserving her fertility.
How common is it?
About 2 percent of all pregnancies are ectopic. Women at risk of having an ectopic pregnancy include those with a history of endometriosis, pelvic inflammatory disease, a prior ectopic pregnancy, or tubal surgery (conceiving after getting your tubes tied carries a 60 percent chance of an ectopic pregnancy). Also included in the at-risk group are those who became pregnant while using progesterone-only birth control pills; women who became pregnant with an IUD in place (though with today’s newer IUDs, especially the hormonal kinds, the chance of an ectopic pregnancy is significantly lower); women with STDs; and women who smoke.
You’ll Want to Know …
More than half of the women who are treated for ectopic pregnancies conceive and have a normal pregnancy within a year.
Ectopic Pregnancy
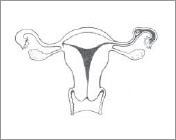
In an ectopic pregnancy, the fertilized egg implants in an area other than the uterus. Here, the egg has implanted in the fallopian tube.
What are the signs and symptoms?
Early symptoms of an ectopic pregnancy include:
Sharp, crampy pain with tenderness, usually in the lower abdomen (it often begins as a dull ache that progresses to spasms and cramps); pain may worsen on straining of bowels, coughing, or moving
Abnormal bleeding (brown spotting or light bleeding that precedes the pain)
If the ectopic pregnancy goes unnoticed and your fallopian tube ruptures, you may experience:
Nausea and vomiting
Weakness
Dizziness and/or fainting
Severe sharp abdominal pain
Rectal pressure
Shoulder pain (due to blood accumulating under the diaphragm)