Fundamentals of Midwifery: A Textbook for Students (74 page)
Read Fundamentals of Midwifery: A Textbook for Students Online
Authors: Louise Lewis

BOOK: Fundamentals of Midwifery: A Textbook for Students
5.31Mb size Format: txt, pdf, ePub
Women are likely to feel some degree of bruising around the vaginal and perineal tissues irre- spective of whether the birth resulted in actual laceration or trauma. The effects of perineal pain can impact on the first experiences of motherhood. It is the responsibility of the midwife to minimize morbidity caused by perineal trauma, promote healing and effectively manage pain.
Hormones
Following delivery of the placenta, oestrogen and progesterone fall to non-pregnant levels within 72 hours of birth (Coad and Dunstall 2011). Oxytocin and prolactin levels are dependent upon lactational demands. Increased prolactin levels during breastfeeding, inhibit follicle stimu- lating hormone (FSH) and luteinizing hormone (LH) release, resulting in lactational amenor- rhoea (see Chapter 12: ‘Contraception and family planning’, for more detail on lactational amenorrhoea).
Haematologic and haemostatic systems
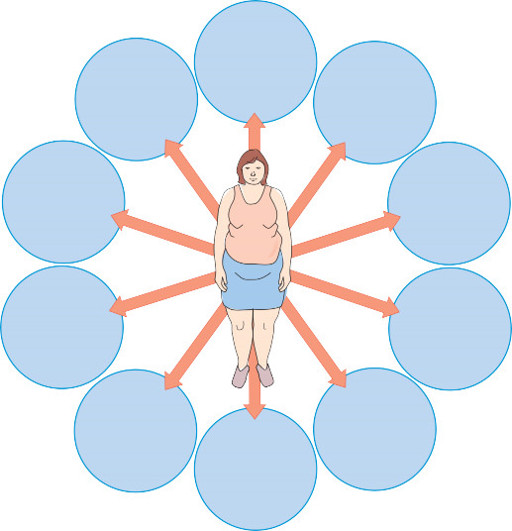
The increased blood and plasma volume during pregnancy results in a physiological hypervol- aemia that allows the woman to tolerate some blood loss after birth, normally 300–500 millili- tres (Coad and Dunstall 2011). Clotting factors increase after delivery due to the removal of the placenta, resulting in a hypercoaguable state in the postpartum period. This predisposes women to the increased the risk of thromboembolic disorders, being the major cause of maternal death identified in previous Confidential Enquiries into Maternal Deaths (2007). Figure 8.1 highlights the risk factors for thromboembolic disorders in women.
Cardiovascular system
The birth of the baby, placenta and membranes, amniotic fluid and loss of blood; results in dramatic maternal haemodynamic changes rendering the cardiovascular system transiently unstable during the immediate postpartum period (Coad and Dunstall 2011). During the first week after the birth, body fluid is mobilised and excreted leading to a decrease in circulating blood volume as haemoconcentration occurs and the components of blood return to normal (Jackson 2011).

169
Critical care admission
Reduced mobility for three or more days, including caesarean section
births Aged over 35 years

170
Pre-existing disease
e.g. thrombophillia. Personal or family history of venous theomboembolism
Obesity – pre pregnancy or early pregnancy BMI of over 30kg/m
2
Significant medical disorders
Multiple pregnancy
Pregnancy-related risk factors including: ovarian hyperstimulation, hyperemesis gravidarum,
pre-eclampsia
Postpartum haemorrhage or blood transfusion
Dehydration
Varicose veins with phlebitis
Figure 8.1
Women at risk of venous thromboembolism.
Renal system
Rapid diuresis occurs particularly during days 2–5 postpartum as the sodium and water reten- tion of pregnancy is reversed (Azulay Chertok 2013). Fluid and electrolyte balance is generally restored to non-pregnant homeostasis by 21 days (Coad and Dunstall 2011). It is important the midwife ensures the woman passes an adequate amount of urine within 6 hours following birth (NICE 2006).
Respiratory system
There is immediate reduction in intra-abdominal pressure when the baby is born, allowing expansion of the diaphragm. Respiratory rate returns to normal within 1–3 weeks (Coad and Dunstall 2011).
Gastrointestinal system
The effect of progesterone reduces gastrointestinal muscle tone and relaxes the abdomen, increasing the likelihood of constipation following birth. The first bowel movement usually occurs within 2–3 days postpartum, but may be complicated by the presence of haemorrhoids (Coad and Dunstall 2011).
Thermoregulation
Transient maternal temperature elevations due to the stress of labour and dehydration can occur following a normal birth which may resolve spontaneously and can be non-infectious. However, women should be monitored closely in the postpartum period, because deviations from the normal may indicate infection (Coad and Dunstall 2011).
Immediate postnatal period
In the United Kingdom (UK) the day of birth is always classified as Day 0, and is important in
relation to the timing for the newborn blood spot screening (see Chapter 9:‘Care of the newborn’, where neonatal screening is discussed in greater depth). The definition of the day of birth varies internationally; some areas define the day of birth as day 0 and in other countries it depends on the time of the day the baby is born. In terms of assessing the health of the newborn in relation to establishing feeding, monitoring sufficient milk intake or jaundice levels, it is advis- able to consider how many hours old the baby is.
Either in the home, midwifery-led unit or hospital environment, immediate postnatal care is guided by an evidence-based approach to care (NICE 2006; 2013). The immediate postnatal period is defined as the first one to two hours after birth; the aim during this period is to support the physiological recovery of the mother, transition to motherhood and support the newborn’s transition to extra uterine life (Dixon 2013). Assessment of the woman’s physiological wellbeing is a crucial part of this period and includes the following assessment; any deviations from the normal would require urgent, immediate medical review.
Postnatal examination of the WOMAN by the midwife
W
Wound assessment – Observe and evaluate for infection and adequate wound healing of the perineum and caesarean section wounds.
O
Observations – Temperature, pulse, respirations and blood pressure.
M
Measure and record first void of urine (should be within 6 hours of birth: NICE 2006).
A
Assessment of the uterus – In the absence of abnormal vaginal loss, or signs of endometritis, assessment of the uterus by abdominal palpation as a routine observation is unnecessary (NICE 2006). Abdominal palpation should be undertaken if a woman has abnormal, excessive or offensive vaginal loss, abdominal tenderness, or fever. Any abnormalities detected, includ- ing in the size, tone and position of the uterus, must be evaluated urgently by a medical practitioner.
N
Note the colour and circumference of the lower limbs and presence of any calf pain – observe and assess for deep vein thrombosis (DVT), although more than 50% of DVTs can be asymp- tomatic (Day 2003; Meetoo 2010).
Monitoring the baby’s health and wellbeing is also a fundamental role of the midwife in the postnatal period (see Chapter 9: ‘Care of the newborn’, where examination of the newborn baby is discussed in greater depth).

171
172
Postnatal examination of the NEWBORN by the midwife
N
Note the baby’s skin colour – should be pink and warm or normal colour for their ethnicity. Any jaundice within the first 24 hours is pathological, and requires immediate review by paediatrician (see Chapter 9: ‘Care of the newborn’, where neonatal jaundice is discussed in greater depth).
E
Elimination – assess adequate passing of urine and stools. Babies who have failed to pass either urine or meconium within the first 24 hours need immediate review by the paediatri- cian. Evaluation of normal elimination patterns is part of the ongoing infant feeding assess- ment and baby’s general wellbeing.

W
Weight loss – within normal parameters within the first few days (not more than 10% of birth weight)
B
Behaviour – the baby should have periods of alertness, normal sleep patterns, waking for regular feeds, normal muscle tone, should lustily cry and be responsive to handling.
O
Observations – should fall within normal ranges; respiratory rate 30–60 breaths per minute, heart rate 100–160 beats per minute, temperature of around 37°C (NICE 2006). Oral mucus membranes should be moist and pink with no evidence of oral
Candida albicans
(thrush), ankyloglossia (tongue tie) or abnormalities with the palate.
R
Rashes – assess for any skin rashes, lesions, birth marks or spots. Attention should also be given to mother’s previous medical history for risk factors such as group B streptococcus.
N
Note the frequency, duration of breastfeeding and effective milk transfer. If formula feeding note the frequency, amount taken and type of formula milk used. Ensure parents are fully informed about the safe preparation of formula milk. (see Chapter 10: ‘Infant feeding’; where feeding is explored in greater depth).
Other books
BlowOuttheCandles by Karenna Colcroft
The Sentinel by Jeremy Bishop
The Devil in Montmartre by Gary Inbinder
The Hobgoblin of the Redwoods by Trevor Scott
Unthinkable (Berger Series) by Brayfield, Merinda
Empty Streets by Jessica Cotter
Foreign Land by Jonathan Raban
This Duke is Mine by Eloisa James
boystown by marshall thornton
An Evening At Gods by Stephen King