How We Die (5 page)
Authors: Sherwin B Nuland

Eventually, about 50 to 60 percent of people with ischemic heart disease will die within an hour of one of their attacks, whether the first or a later one. Since 1.5 million Americans suffer a myocardial infarction each year (70 percent of which occur in the home), it is not difficult to understand why coronary heart disease is America’s biggest killer, as it is in every industrialized country of the world. Almost all of those who survive every infarction will eventually be claimed by the gradual weakening of the heart’s ability to pump.
When all natural causes are taken into account, approximately 20 to 25 percent of Americans die suddenly, defined as unexpected death within a few hours of onset of symptoms in persons neither hospitalized nor homebound. And of these deaths, 80 to 90 percent are cardiac in origin, the remaining segment being due to diseases of the lungs, central nervous system, or the vessel into which the left ventricle pumps its blood, the aorta. When the death is not only sudden but instantaneous, there are only a few that are not the result of ischemic heart disease.
The victims of ischemic heart disease are betrayed by their eating and their smoking and their inattention to such simple housekeeping chores as exercise and the maintenance of normal blood pressure. Sometimes pedigree alone gives them away, in the form of family history or diabetes; sometimes it is that driving impetuosity and aggressiveness that today’s cardiologists call the Type A personality. In a way, the person whose heart muscle will be anguished by angina is very like the overly ambitious schoolchild who throws a hand aggressively into the air when the teacher looks for volunteers—“Choose me, choose me; I can do it better than anyone else!” He is easy to identify, and death will single him out. There is little randomness in the choices made by cardiac ischemia.
Long before we knew about the lurking perils of cholesterol, cigarettes, diabetes, and hypertension, the medical world was beginning to recognize specific characteristics in those persons who seemed destined for cardiac death. William Osler, the author of America’s first great textbook of medicine in 1892, might have been describing James McCarty when he wrote, “It is not the delicate neurotic person who is prone to angina, but the robust, the vigorous in mind and body, the keen and ambitious man, the indicator of whose engines is always at ‘full speed ahead.’ “By their speedometers shall ye know them.“
Despite all medical advances, there are still plenty of people who die with their first heart attack. Like lucky Lipsiner, most of them do not actually suffer death of cardiac muscle but are victimized by a rhythm suddenly made disorderly by the effect of ischemia (or sometimes local chemical changes) on an electrical conduction system already sensitized by a previous injury, whether it was recognized or not. But the usual way in which people succumb to ischemic heart disease these days is not the way of Lipsiner or McCarty. Decline is most often gradual, with plenty of warnings and much successful treatment before the final summons. The killing off of increments of heart muscle takes place over a period of months or years, until that besieged and enervated pump simply fails. It then gives up, for lack of strength or because the command system that controls its electrical coordination can no longer recover from yet another breach of its authority. Those laboratory doctors who are convinced that medicine is a science have accomplished so much that those bedside doctors who know it is an art can often, by careful timing and skillful choice of what is now available to them, provide victims of heart disease with long periods of improvement and stable health.
The fact remains, however, that each day fifteen hundred Americans will die of cardiac ischemia, whether its course has been sudden or gradual. Although preventive measures and modern methods of treatment have been reducing the figure steadily since the mid-1960s, it is virtually impossible for any slope of decline to change the picture for the vast majority of those who carry the diagnosis today or in whom it will be made in the next decade. This unforgiving sickness, like so many other causes of death, is a progressive continuum whose ultimate role in our planet’s ecology is the quenching of human life.
In order to make clear the sequence of events that leads to the gradual loss of a heart’s ability to pump effectively, it is first necessary to review some of the wondrous qualities that enable it to perform with such extraordinary precision when it is healthy. This will be the subject of the first pages of the chapter that follows.
II
A Valentine—and How It Fails
A
S EVERY CHILD
knows, the heart is shaped very much like a valentine. It is made almost entirely of muscle, called myocardium, wrapped around a large central space that is subdivided into four chambers: A vertical front-to-back wall of tissue, called the septum, separates the large space into right and left portions, and a transverse sheet at right angles to the septum divides each of those portions into upper and lower parts, making four in all. Because they have a certain degree of independence from one another, the portions on either side of the vertical septum are often called the right and left heart. On each side, the transverse sheet separating top from bottom is perforated by a central opening fitted with a one-way valve that allows blood to pass easily from the upper chamber (called the atrium) down into the lower chamber (the ventricle). In a healthy heart, the valves close tightly when the ventricle is filled, to prevent blood from regurgitating back up into the atrium. The atria are primarily receiving chambers, and the ventricles are pumping chambers. Consequently, the portion of the cardiac muscle around the upper part of the heart does not have to be as thick as that of the more powerful ventricles below them.
S EVERY CHILD
knows, the heart is shaped very much like a valentine. It is made almost entirely of muscle, called myocardium, wrapped around a large central space that is subdivided into four chambers: A vertical front-to-back wall of tissue, called the septum, separates the large space into right and left portions, and a transverse sheet at right angles to the septum divides each of those portions into upper and lower parts, making four in all. Because they have a certain degree of independence from one another, the portions on either side of the vertical septum are often called the right and left heart. On each side, the transverse sheet separating top from bottom is perforated by a central opening fitted with a one-way valve that allows blood to pass easily from the upper chamber (called the atrium) down into the lower chamber (the ventricle). In a healthy heart, the valves close tightly when the ventricle is filled, to prevent blood from regurgitating back up into the atrium. The atria are primarily receiving chambers, and the ventricles are pumping chambers. Consequently, the portion of the cardiac muscle around the upper part of the heart does not have to be as thick as that of the more powerful ventricles below them.
In a sense then, we have not one heart but two, attached side by side to each other by the septum; each has an upper chamber to receive and a lower one to pump. The two hearts have quite different jobs to do: The function of the right is to receive “used” blood returning from the tissues and drive it the short distance through the lungs, where it will be freshly aerated with oxygen; the left heart, in turn, receives the oxygen-rich blood returning from the lungs and forcefully pumps it out to the rest of the body. In recognition of this division of labor, physicians for centuries have differentiated between the two routes of blood by calling them the lesser and greater circulations.
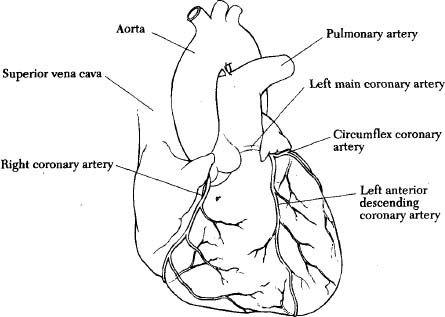
Exterior of a normal adult heart showing the coronary arteries
Diagrammatic section cut through a normal heart with arrows indicating the blood flow
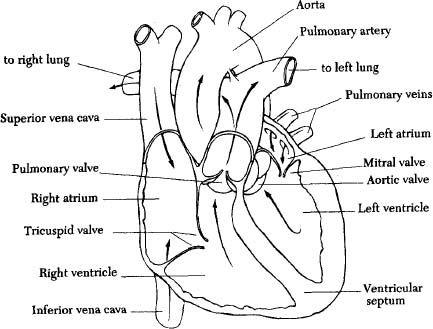
A complete cycle begins with the two large veins that receive dark oxygen-poor blood from the upper and lower portions of the body; the capaciousness, sources, and relative positions of these two broad blue vessels are reflected in the names given them by Greek physicians more than 2,500 years ago: the superior and the inferior vena cava. The two cavae empty their blood into the right atrium, whence it passes down through the valved opening (the right atrioventricular, or tricuspid, valve) into the right ventricle, which pumps it with a pressure equal to the weight of a column of mercury approximately thirty-five millimeters high into a large vessel called the pulmonary (Greek
pulmone
, “lungs”) artery, which soon divides into separate conduits leading into each lung. Revitalized in the lungs by oxygen filtered through microscopic air sacs (called
alveoli
, Latin for “small basins or compartments”), the now bright red blood completes the lesser circulation by returning via the pulmonary veins to the left atrium, to be channeled down into the ventricle and thence driven throughout the body, to the most remote living cell in the great toe.
pulmone
, “lungs”) artery, which soon divides into separate conduits leading into each lung. Revitalized in the lungs by oxygen filtered through microscopic air sacs (called
alveoli
, Latin for “small basins or compartments”), the now bright red blood completes the lesser circulation by returning via the pulmonary veins to the left atrium, to be channeled down into the ventricle and thence driven throughout the body, to the most remote living cell in the great toe.
Because it takes a pressure of approximately 120 millimeters of mercury to generate such a forceful squeeze, the left ventricle’s muscle is more than half an inch wide, giving it the strongest and thickest wall of all four chambers. Pushing out about 70 milliliters of blood (2
⅓
ounces) with each contraction, this vigorous pump drives some 7 million milliliters (more than 14,000 pints) each day, in 100,000 rhythmic and powerful beats. The mechanism of a living heart is a masterpiece of nature.
⅓
ounces) with each contraction, this vigorous pump drives some 7 million milliliters (more than 14,000 pints) each day, in 100,000 rhythmic and powerful beats. The mechanism of a living heart is a masterpiece of nature.
This complicated series of events requires intricate coordination, which is accomplished by messages sent out along microscopic fibers that originate from a tiny ellipse-shaped clump of tissue near the top of the right atrium, in its back wall very close to the entrance of the superior vena cava. It is at this very spot, where the cava empties into the atrium, that the blood starts out on its circuitous journey through the heart and lungs, and there could be no more appropriate point to position the source of the stimulus that makes it all happen. This little bit of tissue, called the sinoatrial (or SA) node, is a pacemaker that drives the coordinated beating of the heart. A bundle of fibers carries the SA node’s messages to a relay station lying between the atria and ventricles (and therefore called the atrioventricular, or AV, node), and from there they are transmitted to the muscle of the ventricles via an arborizing network of fibers called the bundle of His, named for its discoverer, a nineteenth-century Swiss anatomist who spent most of his career at the University of Leipzig.
The SA node is the heart’s personal internal generator; nerves from outside may affect the rate of beating, but it is the conduction of electricity from the SA node that determines the wondrous regularity of its faultless rhythm. Awestruck anew each time they viewed the proud independence of an exposed animal heart, wise men of ancient civilizations proclaimed that this supernal mechanism of boldly autonomous flesh must be the dwelling place of the soul.
The blood within the heart’s chambers is only passing through; it does not stop to nourish the muscular valentine whose syncopated strokes are busily squeezing it along its way through the circulation. For the sustenance required for its forceful labors, the heart muscle, or myocardium, is supplied by a group of separate and distinct vessels, which, because they originate in encircling arteries that wind around the heart like a crown, are called coronary. Branches of the main coronary arteries descend toward the valentine’s tip, giving off twiglike branchlets that bring bright red oxygen-rich blood to the rhythmically heaving myocardium. In health, these coronary arteries are the friends of the heart; when they are diseased, they betray it at its most needful moments.
So commonly do the coronary arteries betray the heart whose muscle they are meant to sustain, that their treachery is the cause of at least half of all deaths in the United States. These “now I love you, now I don’t” vessels are gentler to the gentle sex than they are to those who have more commonly gone out to hunt and fish—not only is infarction less common in women, it tends also to come later in life. The average age of the first infarction of women is in the mid-sixties, but men are more likely to have that terrifying experience ten years earlier. Although the coronary arteries have by that age reached the critical degree of narrowing necessary to threaten the viability of heart muscle, the process begins when its victims are much younger. An oft-quoted study of soldiers killed in the Korean War revealed that some three-quarters of these young men already had some arteriosclerosis in their coronary vessels. Varying degrees of it can be found in virtually every American adult, having begun with adolescence and increasing with age.
The obstructing material takes the form of yellowish white clumps called plaques, which are densely adherent to the inner lining of the artery and protrude into its central channel. The plaques are made up of cells and connective tissue, with a central core composed of debris and a common variety of fatty material called lipid, from the Greek
lipos
, meaning “fat” or “oil.” Because so much of its structure is lipid, a plaque is called an atheroma, from the Greek
athere
, meaning “gruel” or “porridge,” and
oma
, signifying a growth or tumor. The process of atheroma formation being by far the most common cause of arteriosclerosis, it is usually referred to as atherosclerosis, hardening by atheroma.
lipos
, meaning “fat” or “oil.” Because so much of its structure is lipid, a plaque is called an atheroma, from the Greek
athere
, meaning “gruel” or “porridge,” and
oma
, signifying a growth or tumor. The process of atheroma formation being by far the most common cause of arteriosclerosis, it is usually referred to as atherosclerosis, hardening by atheroma.
Other books
Murder at Maddleskirk Abbey by Nicholas Rhea
Moonscatter by Jo Clayton
Balustrade by Mark Henry
Tea-Totally Dead by Girdner, Jaqueline
Journey of Honor A love story by Hawkes, Jaclyn M.
The Mind Pool by Charles Sheffield
The Salt Road by Jane Johnson
The Glass Wall (Return of the Ancients Book 1) by Madison Adler, Carmen Caine
Highlander's Touch by Knight, Eliza
Impossible End (Unchecked Book 3) by Bartel, Sybil