i bc27f85be50b71b1 (53 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

172
ActITE CARE HANDBOOK FOR PHYSICAL THERAPISTS
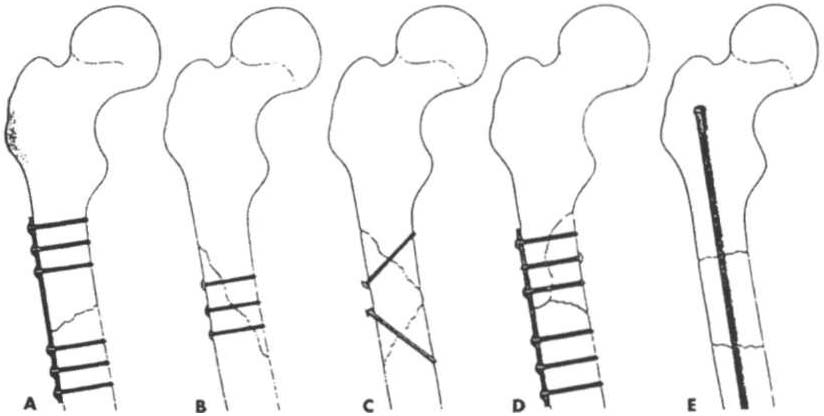
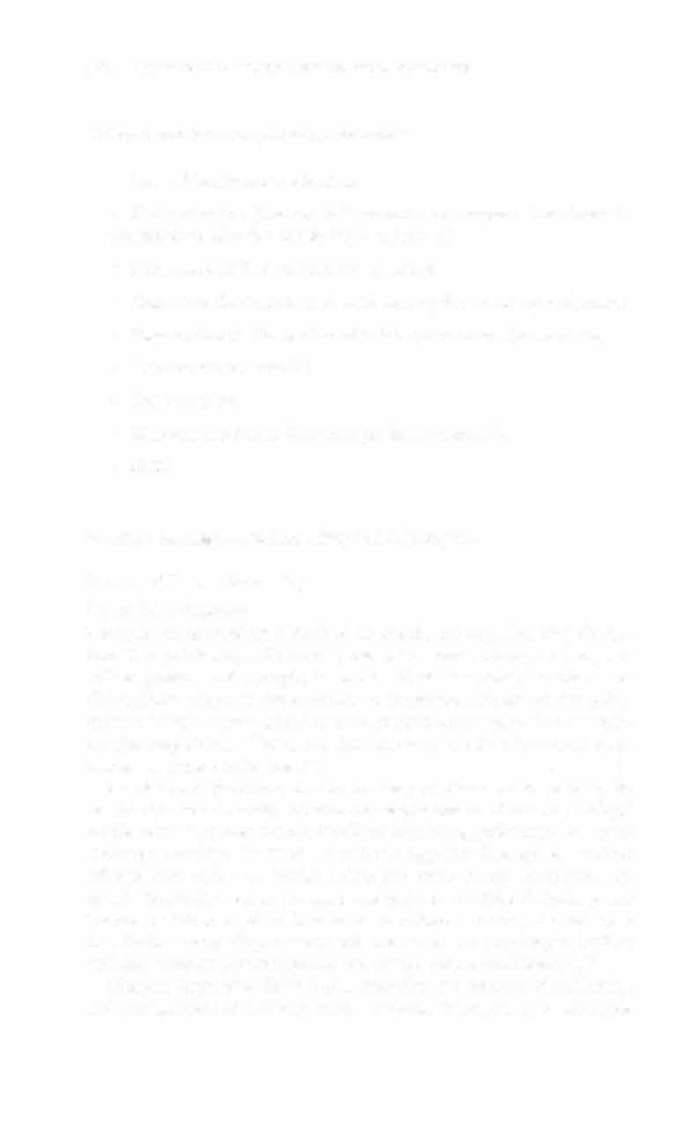
Figure 3-2. Techniques of if/temal fixatiofl. A Plate af/d six screws for transverse or short oblique fracture. B. Screws for [ollg oblique or spiral fracture.
c. Screws for long butterfly fragment. D. Plate and screws for short butterfly
fragment. E. Medullary nail for segmental fracture. (\Vith permission from
PC Beare, JL Myers [eds[. Adult Health Nursing [3rd edt. St. Louis: Mosby,
1 998; 1243.)
when closed methods cannot maintain adequate fixation throughout
the healing phase. Immobilization of the fracture is required to maintain reduction and viability of the fracture site. Immobilization is accomplished through noninvasive (casts or splints) or invasive
(screws, plates, rods, pins, and external fixators) techniques. Regardless of the method of immobilization, the goal is to promote bone healing.
Bone healing occurs in four stages: (1) hematoma formation within
72 hours, (2) fibrocartilage formation in 3 days to 2 weeks, (3) procallus formation in 3-10 days, and (4) remodeling or permanent callus formation in 3-10 weeks.S I,O Table 3-4 lists the multitude of factors that contribute to the proper or improper healing of bone and
affect the time frames for healing.
Complicatio/IS of Fracture
Complications of fracrure may be immediate (within days), delayed
(weeks to months), or late (months to years). The immediate or early


MUSCULOSKELETAL SYSTEM 173
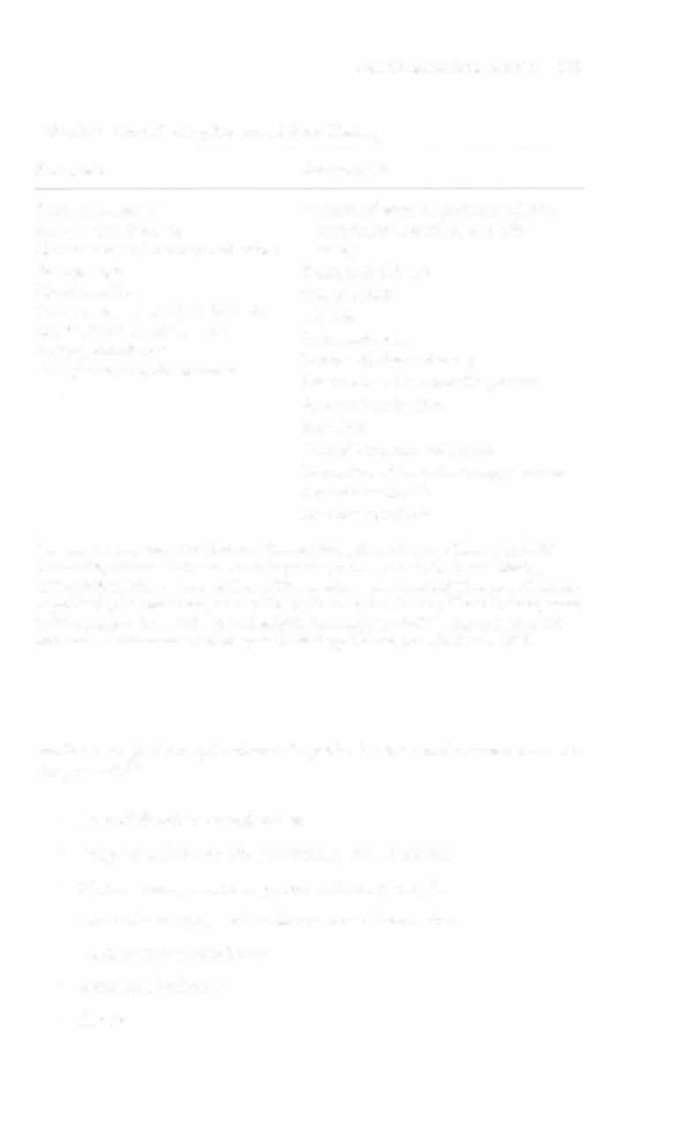
Table 3-4. Contributing Factors of Bone Healing
Favorable
Unfavorable
Early mobilization
Presence of disease, such as diabetes,
Early weight bearing
anemia, neuropathy, or malig
Maintenance of fracture reduction
nancy
Younger age
Vitamin deficiency
Good nutrition
Osteoporosis
Distal or proximal shaft fracture
Infection
Minimal soft tissue damage
Irradiated bone
Patient compliance
Severe soft tissue damage
Presence of growth hormone
Distraction of fracture fragments
Severe comminution
Bone loss
Multiple fracture fragments
Disruption of vascular supply to bone
Avascular necrosis
Corticosteroid use
Sources: Adapted from CA Christian. General Principles of Fracture Treatmem. In ST
Canale (ed), Campbell's Operative Onhopaedics, Vol. 3 (9th ed). St. Louis: Mosby,
1998;1999;JM Black. Nursing Care of Clients with Musculoskeletal Trauma or Overuse.
In JM Black, E Marassarian·Jacobs (005), Medical·Surgical Nursing Clinical Management
for Continuity of Care (5th ed). Philadelphia: Saunders, 1997;2134; and data from LN
McKinnis. Fundamentals of Orthopedic Radiology. Philadelphia: FA Davis, 1997.
medical-surgical complications of special interest in the acute care setting inciudelO
• Loss of fixation or reduction
• Deep vein thrombosis, pulmonary or fat emboli
• Nerve damage, such as paresthesia or paralysis
• Arterial damage, such as blood vessel laceration
• Comparrment syndrome
• Incisional infection
• Shock


174 AClITE CARE HANDBOOK FOR I)HYSICAL THERAPISTS
Delayed and late complications include'o
• Loss of fixation or reduction
•
Delayed IInion (fracture fails ro unite in a normal time frame in
the presence of unfavorable healing factors)
•
NOllullioll (failure of fracture to unite)
•
Malunion (fracture healed with an angular or rotary deformity)
•
Pseudarthrosis (formation of a false joint at the fracture site)
•
Post-traumatic arthritis
•
Osteomyelitis
•
Myositis ossi{icalls (heterotropic bone in muscle)
• AVN
Frachtre Managemellf According fo Body Regioll
Pelvis and Lower Extremity
Pelvic Ring Fracture
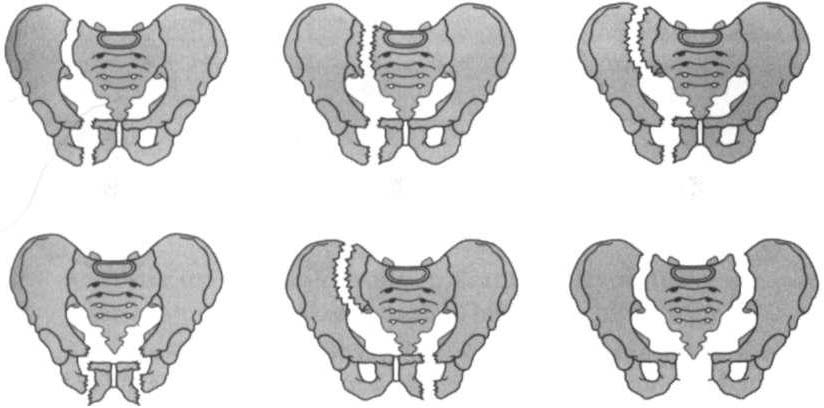
Pelvic fracture stability is defined by the degree of pelvic ring disruption. The pelvic ring is formed by the paired coxal bones, sacrum, sacroiliac joints, and symphysis pubis. UlIslable pelvic fractures or dislocations occur in the anterior or posterior column of the pelvis
owing to high-impact lateral or anteroposterior compression, or vertical shearing forces.) There is a disruption of the ring in two or more places, as shown in Figure 3-3.
Stable pelvic fractures, due to low-impact direct blows or falls, do
nOt involve or minimally involve the displacement of the pelvic ringJ
Stable pelvic fractures include localized iliac wing, pubic rami, or sacral
fractures. Avulsion fractures of anterior superior iliac spine, anterior
inferior iliac spine, or ischial tuberosity from strong contraction of
muscle (rypically seen in younger athletes) are considered stable pelvic
fractures7 When a pelvic fracture is described as stable, it is inherent
that further bony displacement will not occur on physiologic loading
and that invasive procedures are not needed before mobilization."
Chapter Appendix Table 3-A.l describes the fracture classification
and management of pelvic fractures. External fixation is used for stable