Pediatric Primary Care (107 page)

I. Follow up.
1. Per orthopedics.
2. Patients will be followed long term, bed rest with traction, bracing, and surgery performed as indicated.
J. Complications.
| Degenerated changes, 721.9 |
| Unstable gait, 781.2 |
1. May not show on initial films.
2. Delayed treatment affects normal growth of hip joint.
3. Residual deformities (coax magna), limited range of motion, unstable gait, pain, early degenerated changes seen with treated and untreated.
K. Education.
1. Progressive until body replaces “dead” femoral head with new bone; younger it occurs, longer body has to replace collapsing bone and remodel femoral head.
2. No pressure should be put on rebuilding bone, but should be able to move in joint for shaping.
X. HIP PAIN: SLIPPED CAPITAL FEMORAL EPIPHYSIS
| Slipped capital femoral epiphysis, 732.2 |
A. Femoral neck “slips” (displaces anteriorly) at physis (growth plate), leaving femoral head behind in acetabulum
(
Figure 30–6
).
B. Etiology.
1. Unknown; however, suspect multifactorial cause, biomechanical, obesity, endocrine, metabolic, trauma, genetics, and other causes (e.g., kidney disorders or radiation).
C. Occurrence.
1. Most common hip disorder of adolescents, 3 of 100,000 are 8–17 years of age.
2. Males (10–17 years of age) affected 2–3 times more often than females (8–15 years of age).
3. Left hip most often affected; bilateral 25–70%.
D. Clinical manifestations.
1. Hip, groin, medial thigh, knee pain; sometimes for months.
2. May be brought on by very minor trauma (chronic/acute or acute on chronic).
3. Antalgic gait (limp to keep weight off painful extremity) or inability to bear weight.
Figure 30–6
Slipped capital femoral epiphysis. Note the appearance of ice cream falling off the cone.
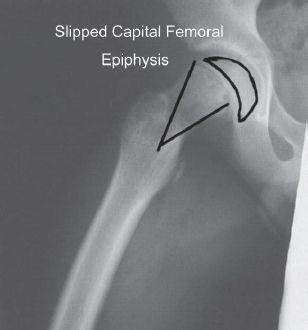
Source:
Courtesy of Miki Patterson.
E. Physical findings.
1. Range of motion may be limited depending on severity of slip, may have limited internal rotation and abduction of the hip.
F. Diagnostic tests.
1. Radiographs AP pelvis and true lateral (not frog lateral because may cause more femoral head displacement).
G. Differential diagnosis.
| Appendicitis, 541 |
| Hip pain, 719.45 |
| Testicular torsion, 608.2 |
1. Knee problem.
2. Infection.
3. Inflammation.
4. Referred pain such as appendicitis, testicular torsion.
5. Other orthopedic conditions or malignancy.
H. Treatment.
1. Immediate referral to orthopedist.
2.
Do not
allow further weight bearing because femoral head can “slip” further.
3. Surgical intervention with “pinning” by screw(s) to fuse physis between femoral head and neck.
I. Follow up.
1. Orthopedics typically allow partial weight bearing with crutches for 6–8 weeks.
2. Return in 2 weeks for wound check, staple removal.
3. Follow healing clinically and radiographically for several months/years.
J. Complications.
| Avascular necrosis, 733.4 |
| Chondrolysis, 733.99 |
| Degenerative changes, 721.9 |
| Malunion, 733.81 |
1. Missed on X-ray 25% of time.
2. Avascular necrosis.
3. Chondrolysis (acute hylan cartilage necrosis).
4. Loss of range of motion.
5. Limb shortening.
6. Early degenerative changes.
7. Malunion.
K. Education.
1. High incidence of recurrence of other hip.
2. Parents or child should report any similar findings and be seen immediately.
XI. KNEE PAIN: OSGOOD-SCHLATTER DISEASE
| Knee pain, 719.46 |
| Osgood-Schlatter disease, 732.4 |
A. Painful swelling of tibial tubercle, caused by traction and resulting in apophysitis.
B. Etiology.
1. Overuse by chronic repetitive knee flexion.
C. Occurrence.
1. 11–14 years of age during rapid growth.
2. Males > females, but ratio changing with increased female participation in sports.
3. Frequently bilateral.
D. Clinical manifestations.
1. Pain with running, jumping, kneeling. Resolves/fades with rest.
E. Physical findings.
1. Pain in anterior knee; warmth, swelling, and tenderness over tibial tubercle, especially with resistive knee extension (kicking motion) or squatting.
F. Diagnostic tests.
1. Radiographs of knee: AP and lateral and 10° obliques to rule out tumor or fracture.
2. Classic prominent tibial tubercle above physis
(
Figure 30–7
).
Figure 30–7
Osgood-Schlatter disease: apophysitis of the tibial tubercle.

Source:
Courtesy of Miki Patterson.
G. Differential diagnosis.
| Knee fracture, 822 |
| Sinding-Larsen-Johansson syndrome, 732.4 |
1. Tumor.
2. Fracture.
3. Sinding-Larsen-Johansson syndrome (apophysitis of distal pole of patella).
H. Treatment.
1. Limit activities, especially sports; ice after activity.
2. Hamstring and quadriceps stretching and strengthening.
3. Knee immobilizer or cylinder casting for brief periods to manage severe pain.
4. Ibuprofen.
I. Follow up.
1. Teach patients, families to decrease activity; wear knee immobilizer when painful.
2. Follow up until skeletal maturity seen in closure of physis or growth plate.
J. Complications.
| Apophysis deformity, 738.9 |
| Enlargement of tibial tubercle, 718.86 |
| Tibia fracture, 823.8 |
1. Enlargement of tibial tubercle (bony prominence).
2. Pain may continue into adulthood.
3. Fracture of tibial tubercle.
4. Premature closure of apophysis causing recurvatum deformity.
K. Education.
1. “Bump” made because body thinks there is injury to bone which is being pulled apart at growth plate by patella; tendon bump will
not
go away.
2. Continued use while painful typically increases size of “bump”; this is cosmetically unappealing for most and may interfere with kneeling. Condition ceases to exacerbate on skeletal maturity.
XII. PHYSIOLOGIC GENU VARUM (BOW LEGS)
| Genu varum, 736.42 |
A. Etiology.
1. Physiologic genu varum or bowing is part of normal development.
Other books
Child of Recklessness (Trials of Strength Book 2) by Matthew R. Bell
See If I Care by Judi Curtin
Bearly A Squeak by Ariana McGregor
The Witches of Barrow Wood by Kenneth Balfour
PRIMAL INSTINCT by JANIE CROUGH
Conversation in the Cathedral by Mario Vargas Llosa
Snow Queen by Emma Harrison
Ready Player One by Cline, Ernest