Pediatric Primary Care (39 page)

a.
Propionibacterium acnes
distend the follicle, causing leakage around the comedone.
b. Lesions developing in the lower portion of the follicle create warm, tender nodules and cysts. These lesions may result in scars, which in turn can develop into keloids.
c. Inflammatory acne lesions may resolve with postinflammatory hyperpigmentation, which usually clears after several months.
D. Physical findings. The highest concentration of sebaceous glands occurs on the face, chest, back, and shoulders. A variety of lesions appear simultaneously, presenting with a variety of comedones, papules, pustules, and nodules. Acne appears to be more severe in winter months, and females report a premenstrual hormonal correlation. The severity of acne is determined by the quantity, type, and distribution of lesions.
E. Diagnostic tests. Acne is a visual diagnosis. History should include family history, other medical disorders, duration of acne, products used, and previous treatments–over-the-counter as well as prescription medications. Physical examination should include grade of acne according to type and location of lesions. See
Table 20-1
. Laboratory testing is indicated only if adrenal or gonadal function are in question.
F. Differential diagnosis.
1. Tuberous sclerosis.
2. Nevus comedonicus.
3. Miliaria of the newborn.
4. Flat warts.
5. Molluscum contagiosum.
Table 20-1
Grading Scale for Acne Severity
| Scale | Definition | |
| 0 | None: skin is clear | |
| 1 | Few comedones | |
| 2 | Mild comedones, few papules, minimal erythema | |
| 3 | Comedones, papules, pustules, erythema | |
| 4 | Moderate comedones, greater number of papules, pustules extending over wider area of face, chest, shoulders, back, increasing erythema | |
| 5 | Comedones, increasing number of papules, pustules, nodules with erythema | |
| 6 | Comedones, papules, pustules, nodules, cysts; scarring may or may not be present with hyperpigmentation |
Table 20-2
Treatment of Acne
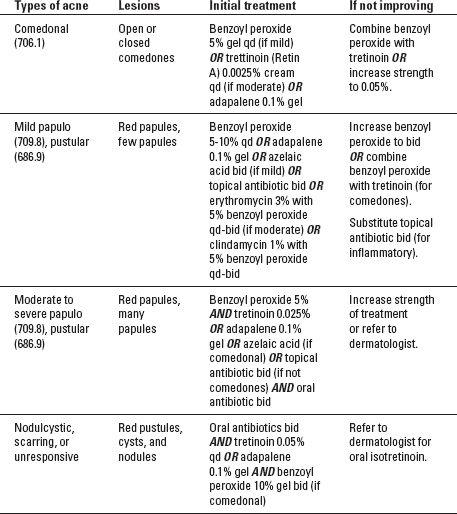
G. Treatment. Goals of treatment include altering keratinization, counteract excess sebum production, decrease the production of
P. acnes
, and minimize scarring. Treatment choices depend on the severity of acne. See
Table 20-2
.
H. Follow up. Acne patients should be evaluated every 3 to 6 months for compliance, treatment progress, and worsening of the disorder. Dermatology referral should be considered for patients who are not 50% improved on topical medications and oral antibiotics after 6 months, or those who are developing scarring from acne lesions. Patients treated with isotretinoin are monitored monthly. The development of the iPLEDGE Program requires providers, patients, and pharmacists to access the program monthly to monitor for pregnancy, blood donation, and contraceptive counseling, as isotretinoin is teratogenic.
I. Complications. Lack of patient motivation, inappropriate treatments, and inappropriate expectations complicate acne treatment. Psychologic effects of acne include poor self-esteem, depression, and problems with interpersonal relationships. Resistance to treatment, especially oral antibiotics, also complicate treatment.
J. Education. Proper use of medications as well as cleansers, moisturizers, and make-up are important to encourage compliance. Although no evidence indicate dietary restrictions are helpful, a well-balanced diet including adequate intake of water is important in treatment. It takes weeks to months to treat acne, and occasionally the disorder will worsen with treatment. Compliance is crucial.
II. BITES
A. Animal bites.
1. Etiology and occurrence. Cat and dog bites, as well as other animal bites, are common injuries.
2. Clinical manifestations. Bite wounds may be infested with
S. aureus
, streptococci, and other oral flora bacteria. Approximately one-third of animal bites contain anaerobic bacteria. It is difficult to predict which wounds will become infected.
3. Physical findings and complications. Injuries include lacerations, crushing injuries, deep puncture wounds, as well as bone, tendon, muscle, and neurovascular tissue damage from deep bites. Secondary infection can lead to cellulitis.
4. Diagnostic tests. Wound cultures identify infectious agents. X-ray and MRI studies reveal bone, vascular, and nerve damage.
5. Differential diagnosis. Identify laceration and puncture wounds from other sources.
6. Treatment. Culture wounds before cleansing and debridement. Antibiotics for infected wounds, management of bone, tendon, nerve, and vascular wounds by appropriate specialists. If suturing is necessary, observe closely for infection. Hospitalization and reconstructive surgery as indicated. Tetanus booster if indicated. Rabies prophylaxis if indicated. Psychological management.
7. Education. Teach children not to provoke any animal. Provide adequate adult supervision of children. Report stray animals to animal control officials.
B. Human bites.
1. Clinical manifestations. Human bite wounds harbor both anaerobic and aerobic bacteria, as well as
S. aureus
and Haemophilus, with a higher incidence of infections and complications than other bites. Human bites include occlusional wounds when teeth are sunk into the skin, and clenched-fist injuries when a tooth penetrates a joint or bone.
2. Diagnostic tests. Radiographic and surgical evaluation if a joint or bone is penetrated. Bacterial cultures for anaerobic and aerobic bacteria.
3. Treatment. Irrigation decreases risk of infection. Debridement of wound edges, appropriate antibiotic treatment (Augmentin, Erythromycin) and immunization if indicated.
4. Complications. Residual disability are frequent after clenched-fist injuries, including abscess, osteomyelitis, tendonitis, tendon rupture, and stiffness of the joint.
C. Atopic dermatitis/eczema.
1. Etiology. Eczema is a chronic disorder characterized by exacerbations and remissions. There is a strong family history of allergies and asthma.
2. Occurrence. Atopic dermatitis, or eczema, is the most common skin disorder seen in children, affecting 10-15% of all children; 30-80% percent of atopic patients continue to experience flares during their lifetime.
3. Physical findings. Atopic dermatitis is characterized by intense pruritus, erythema, scale, and excoriations. The borders are diffuse. Crusting and oozing are common in infants. Thickened skin (lichenification) from persistent scratching and rubbing may be present. Distribution is on the scalp, face, and extensors in infants, on the neck and flexor folds in children, and on the hands and feet in adolescents and adults.
3. Diagnostic tests. Atopic dermatitis is a clinical diagnosis based on careful history and clinical examination. A potassium hydroxide (KOH) scraping will exclude fungal infections.
4. Differential diagnosis. Tinea, seborrheic dermatitis, psoriasis, scabies, and molluscum contagiosum.
5. Treatment. Goals of treatment include controlling itching with antihistamines, hydrating the skin with lukewarm tub soaks followed by application of emollient moisturizers, (Eucerin, Aquaphor) alleviating inflammation with topical corticosteroids, maintaining remission with immunomodulators such as Elidel and Protopic, and treating secondary bacterial infections with appropriate topical and systemic antibiotics. Bleach baths kill microbes that cause infection in children with atopic dermatitis. Add ¼ cup of bleach to a bath tub of lukewarm water and allow the child to soak for 10 minutes, followed by adequate moisturizers. Identifying and treating allergens helps control flares.
5. Follow up. Failure to respond to treatment requires referral to a dermatology specialist. Referral to an allergist may be necessary for evaluation and management of allergies.
6. Complications. Secondary bacterial infections from excoriations include Group A beta-hemolytic streptococci and staphylococcus. Patients with atopic dermatitis have a higher incidence of viral infections, including herpes simplex, molluscum contagiousum, and warts.
7. Education. There is no cure for atopic dermatitis. It is characterized by exacerbations and remissions. Teach proper use of antihistamines, topical corticosteroids, and immunomodulators, as well as bathing followed by application of moisturizers. Identify aggravating factors such as stress, allergies, weather change, and infections.
III. BURNS
A. Etiology and occurrence. Burns can be caused by thermal, chemical, or electrical agents. The majority of burns are thermal, and the minority of burns are chemical. Most burns are minor and can be managed on an outpatient basis.
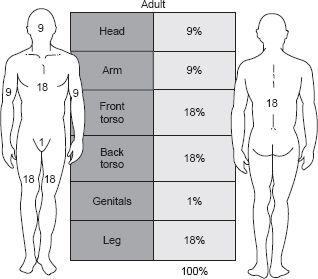
B. Clinical manifestations. Burns are classified by depth of injury. Superficial or first-degree burns involve only the epidermis. Partial thickness or second-degree burns involve damage to the epidermis and varying depths of the dermis. Full thickness or third-degree burns involve the epidermis, the dermis, and the subcutaneous fat. Third-degree burns are painless. The size of the burn is measured by the percent of total body surface area (TBSA) involved. The rule of nines estimates the TBSA. see
Figure 20-1
.
C. Physical findings. Physical examination includes the TBSA, distribution, and depth of involvement.
D. Diagnostic tests. Bacterial cultures for suspected infection. Laboratory evaluation for serious burns includes complete blood count (CBC), serum electrolytes, serum glucose, blood urea nitrogen (BUN), creatinine, and urinalysis.
Figure 20-1
Rule of nines.
Other books
Death of a Stranger by Eileen Dewhurst
One Secret Night by Yvonne Lindsay
Wilderness of Mirrors by Ella Skye
Sabotage Season by Alex Morgan
What Happens in Tuscany... by T A Williams
Semi-Detached by Griff Rhys Jones
Imposter by Chanda Stafford
Wrangling with the Laywer by Fran Louise
Keeping Faith by T.J. Vertigo