Pediatric Primary Care (41 page)

D. Differential diagnosis. Viral exanthems, drug eruption, varicella, disseminated gonococcal infection, and Lyme disease.
E. Treatment. Doxycycline or tetracycline are the drugs of choice. Alternative treatment for those unable to treat or with history of allergies to these drugs include chloramphenicol. Supportive treatment for fever and myalgias.
F. Follow up. Close follow up for complications persisting beyond 1 year after acute infection for neurologic and nonneurologic disabilities.
G. Complications. Death is associated with older patients, those with delay in treatment, or undiagnosed disease. Untreated disease death rate is 25%. Other complications include neurologic disorders including hearing loss, peripheral neuropathy, bladder and bowel incontinence, cerebellar dysfunction, language disorders.
H. Education. Avoidance of tick bites and prompt removal of ticks. No vaccine is available.
X. MOLLUSCUM CONTAGIOSUM
A. Etiology. Molluscum contagiosum is a virus caused by a poxvirus infecting the epidermis, causing white papules. The center of the lesions are filled with keratinous material.
B. Occurrence. Molluscum contagiosum is common in infants and toddlers, and most adults are immune.
C. Clinical manifestations and physical findings. One- to 6-mm discrete umbiliated papules are seen usually in the interiginous areas. Occasionally, larger lesions up to 15 mm may be found. Incubation period is 2-7 weeks. Children are contagious as long as lesions are present. Lesions may resolve spontaneously, but this may take years.
D. Differential diagnosis. Warts, closed comedones, epidermal cysts. Blisters may be confused with molluscum contagiosum.
E. Treatment. Papules may be removed by curette or incision and drainage, however, this procedure is painful and may result in scarring. Treatment with liquid nitrogen, cantharidin, potassium hydroxide, or podophyllin applied to the central umbilication is less traumatic. Topical treatment at home with imiquimod cream is an alternative.
F. Complications. Secondary impetigo. Atopic dermatitis. Scarring.
G. Follow up. Office visits every 2 weeks for treatment will control spread of lesions.
H. Education. Lesions are benign but highly contagious.
XI. WARTS
A. Etiology. Warts are benign virus-induced tumors caused by human papillomavirus (HPV). More than 76 subtypes have been identified and are associated with specific cutaneous and mucous membrane location.
B. Occurrence. Transmission is by direct contact, and infection can occur by autoinnoculation, especially in interiginous areas. Immunocompromised patients are at increased risk.
C. Clinical manifestations and physical findings. Verrucous papules appear as solitary lesions or may be grouped, confluent, flat, or pedunculated. They may appear anywhere on the body, but occur most often on the extremities, interrupting the dermal ridges.
D. Diagnostic tests. No testing is necessary.
E. Differential diagnosis. Plantar warts may be differentiated from calluses by the interruption of dermal ridges. Common and filiform warts present no diagnostic challenge. Flat warts are often confused with closed comedones, lichen planus, and molluscum contagiosum.
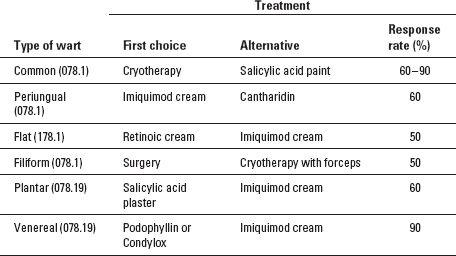
F. Treatment. Multiple therapeutic modalities are available for treatment, including liquid nitrogen, cantharidin, electrodessication, laser therapy, candida and bleomycin injection, and excision. It is unlikely the warts will resolve with a single treatment except excision, and recurrence is high. Warts frequently resolve spontaneously, and good clinical judgment should be exercised when considering various therapies versus cautious observation. Multiple salicylic acid treatments are available over the counter, as well as prescription retinoids, podophyllin, and imiquimod cream. Cimetidine 30-40 mg/kg/day in combination with other treatment modalities is effective for resistant warts. See
Table 20-4
.
G. Follow up. Close follow up every 2 weeks.
Table 20-4
Treatment of Viral Warts
H. Complications. Proliferation of warts resulting in pain or difficulty with daily tasks. Social anxiety and social isolation due to cosmetic embarrassment requires more aggressive treatment.
I. Education. The recalcitrant nature of warts should be emphasized, as well as the need for multiple treatments. Genital warts in infants and toddlers should be evaluated for the possibility of sexual abuse.
XII. FIFTH DISEASE (ERYTHEMA INFECTIOSUM)
A. Etiology and occurrence. Erythema infectiosum (fifth disease) is caused by human parvovirus B19.
B. Clinical manifestations and physical findings. Fifth disease begins with intense red cheeks (“slapped cheeks”) and spreads to involve arms, legs, and trunk with a macular red lacy exanthem. Although initially lasting less than 1 week, with heat exposure the exanthem can recur for up to 4 months.
E. Diagnostic tests. Serum obtained within 30 days of onset of rash will confirm the presence of immunoglobulin M (IgM) B19 antibodies
F. Differential diagnosis. Drug eruptions and other morbilliform eruptions can be differentiated by the classic lacy rash of fifth disease.
G. Treatment. There is no specific treatment nor are there specific control measures, other than avoid exposure to pregnant women and those who are immunocompromised. The disease is no longer contagious once the skin eruption occurs.
H. Complications. Hydrops fetalis may result in pregnant women who have not developed antibodies. Immunocompromised children may develop persistent infection. Patients with transient anemias may develop aplastic crisis and severe anemia.
I. Education. Inform of the likelihood of recurrence with heat exposure, including exercise and sun exposure. Avoid pregnant women and immunocompromised individuals, and those with chronic anemias.
XIII. SEBORRHEIC DERMATITIS
| Atopic dermatitis, 691.8 | Psoriasis, 696.1 |
| Candida infection, 112.9 | Scale, 782.8 |
| Contact dermatitis, 692.9 | Seborrhea dermatitis, 690.1 |
| Infantile seborrhea dermatitis, 690.12 | Tinea, 110 |
A. Etiology. Seborrheic dermatitis is an inflammatory disorder characterized by yellow-waxy scales in the scalp, eyebrows, auricular areas, and interiginous areas. These are areas of active sebaceous glands.
Malasezia furfur
is a yeast found on normal skin but highly prevalent in seborrheic dermatitis.
B. Occurrence. Usually appears in infancy and continues through adolescence and adulthood. More common in males. Affects 2-5% of the population.
C. Clinical manifestations. Greasy scales with well-defined borders, thick adherent symmetrical plaques distributed in the scalp, face, chest, and diaper area.
D. Differential diagnosis. Candidiasis, tinea, psoriasis, perioral dermatitis, as well as discoid lupus erythematosus.
E. Treatment. Removal of scalp scale with mineral oil and a fine tooth-comb provides relief. Shampoos containing selenium sulfide, pyrithione zinc, or ketaconazole can be used on the scalp as well as a face and body wash twice weekly as needed. Mild topical corticosteroids used sparingly control pruritus and erythema. In children older than 2 years of ages, topical immunomodulators may be used in place of topical steroids.
F. Education. This disorder waxes and wanes, therefore patients should be educated to restart therapy at the first sign of recurrence.
XIV. ERYTHEMA TOXICUM NEONATORUM
| Erythema toxicum, 778.8 | Pyoderma, 686 |
| Herpes simplex, 054.9 | Skin disorder, 709.9 |
A. Etiology. A common benign, self-limited eruption in the healthy, full-term newborn. Correlated with birth weight and gestational age, and seldom seen in preterm infants.
B. Occurrence. 30-70% full-term newborns, affecting sexes and races equally.
C. Clinical manifestations. One- to 2-mm discrete, pale yellow papules and pustules surrounded by erythematous wheal, predominantly on the face, trunk, and proximal extremities.
D. Diagnostic tests. Clinical appearance. Microscopic examination with Gram stain or Wright stain of pustular contents shows predominance of eosinophils.
E. Differential diagnosis.
| Congenital cutaneous candidiasis, 112.9 | Miliaria rubra, 705.1 |
| Cytomegalovirus, 771.1 | Scabies, 133 |
| Group A streptococcal infection, 041.01 | Superfi cial staphylococcal |
| Herpes simplex, 054.9 | infection, 041.11 |
F. Treatment. No treatment necessary.
G. Education. Reassure parents that this is transient and benign. Postinflammatory hyperpigmentation may follow but resolves within weeks to months.
XV. PITYRIASIS ROSEA
| Pityriasis rosea, 696.3 | Psoriasis, 696.1 |
| |
A. Etiology. Common, benign, self-limited rash characterized by solitary salmoncolored “herald patch” which precedes exanthema by 1 to several weeks. Lesions usually asymptomatic. Human herpes virus types 6 and 7 have been implicated but not proven in etiology.
B. Occurrence. 10-35 years. Rare under 2 years of age. Most common in fall and spring of the year.
C. Clinical manifestations. Herald patch 1-10 cm followed by smaller, salmon-colored plaques with a fine collarette of scale, follows skin lines in a “Christmas tree configuration.” Headache, malaise, and pharyngitis precedes rash in <5% of cases.
D. Physical findings. Lesions on the trunk most common, in the axillae, posterior trunk, inguinal areas. Less common on the arms and legs. The face and head typically spared.
E. Diagnostic tests. Usually a clinical diagnosis based on history and clinical appearance. A KOH may be performed to rule out tinea.
F. Differential diagnosis.
| Inea versicolor, 111 | Tinea corporis, 100.5 |
| Psoriasis, 696 | |
G. Treatment. No treatment is necessary, as this condition is self-limited. If lesions are pruritic, mild topical corticosteroids applied sparingly to affected areas as well as antihistamines control itching.
H. Education. Stress the benign nature of the exanthema. Post-inflammatory hyperpigmentation in pigmented skin can occur, and should be protected from sun exposure. Hyperpigmentation will resolve with time. It is uncommon for pityriasis rosea to recur.
BIBLIOGRAPHY
Burkhart CN, et al.
Visual DX: Essential Pediatric Dermatology.
Philadelphia, PA: Lippincott Williams & Wilkins; 2010.
Other books
The Influence by Ramsey Campbell
Nail Biter by Sarah Graves
The Girl in the Comfortable Quiet by Susan Ward
Libby on Wednesday by Zilpha Keatley Snyder
Breakheart Pass by Alistair MacLean
Taydelaan by Rachel Clark
The Summer House by Jean Stone
Cast Iron Conviction (The Cast Iron Cooking Mysteries Book 2) by Jessica Beck
Having Adam's Baby (Harlequin Special Edition) by Butler, Christyne
Set Free by Anthony Bidulka