Pediatric Primary Care (49 page)

8. The groups most at risk for DRSP are:
a. Children younger than 24 months of age.
b. Those who have recently received beta-lactam drugs, were recently treated with antibiotics, and/or had a recent ear infection.
c. Children exposed to large numbers of other children (e.g., daycare attendance in children 2 months to younger than 5 years of age, or household crowding in children older than 2 years of age).
d. Those with immune deficiencies (e.g., sickle cell disease, HIV, malignancy). The proportion of penicillin-resistant
S. pneumoniae
strains may be 40-50% and half of these may be highly resistant.
B. Occurrence.
1. After upper respiratory infection (URI), OM most common disease of childhood; peak prevalence from 6 to 36 months of age. Incidence declines at about 6 years of age.
2. Incidence has dramatically increased since 1985; greatest in children younger than 2 years of age.
3. By 3 years of age, most have had at least 1 acute infection; 33% have had 3.
4. Those with first episode early in life have increased risk for developing chronic ear disease.
5. More common in boys than in girls.
6. Caucasians, Native Alaskans, Native Americans have higher incidence than African Americans.
7. More frequent in low-income and large families and those children in group daycare settings.
8. Those immunocompromised, including those with AIDS, have higher incidence.
9. Smoking in household increases incidence.
10. Bottle-fed infants have higher incidence than breastfed infants.
11. Incidence, prevalence of otorrhea: tympanostomy tubes in place longer.
C. Clinical manifestations.
1. Diagnosis of AOM requires:
a. History of acute onset of signs and symptoms.
b. Presence of middle ear effusion.
c. Signs and symptoms of middle ear inflammation.
d. Distinct erythema of TM or distinct otalgia (discomfort clearly related to the ear[s] that causes sleep disturbances and/or interferes with normal activity).
2. Most common younger than 2 years of age.
3. Acute onset of ear pain and fever; pulling, tugging, rubbing at infected ear.
4. Occasionally asymptomatic.
5. Fever in 50% of cases.
6. Other associated symptoms: irritability, disturbed sleep, restlessness, rhinorrhea or URI, cough, malaise, sore throat, stiff neck, refusal of bottle, change in eating habits, vomiting, diarrhea.
7. May report recent URI, previous ear infections, allergies, taking bottle to bed, infant supine when feeding from bottle, attending daycare, other siblings sick.
8. Hearing loss.
D. Physical findings.
1. Fever is common.
2. Signs of URI or allergies.
3. Possible red, enlarged tonsils (pharyngitis).
4. Cervical nodes often enlarged.
5. Otoscopic findings: Middle ear effusion must be present as evidenced by any of the following: bulging TM, decreased or absent mobility of the TM as noted with pneumatic otoscopy, air fluid level behind the TM, otorrhea reflectometry.
E. Diagnostic tests.
1. Pneumatic otoscopy to assess mobility of TM.
2. Tympanometry: to supplement but not replace pneumatic otoscopy, for children older than 6 months of age.
3. Acoustic reflectometry.
4. Tympanocentesis with culture and sensitivity testing is diagnostic of organism.
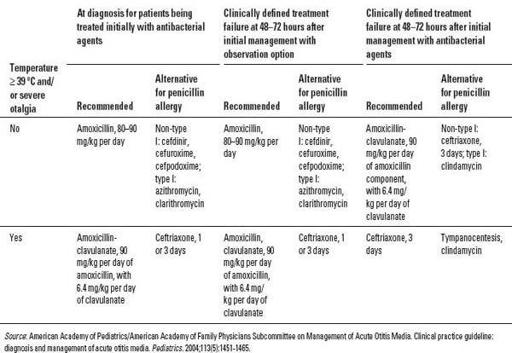
Table 22-1
Recommended Antibacterial Agents for Patients Who Are Being Treated Initially with Antibacterial Agents or Have Failed 48 to 72 Hours of Observation or Initial Management with Antibacterial Agents
F. Differential diagnosis.
| Dental abscess, 522.5 | Mastoiditis, 389.3 |
| Dysfunction 524.6 | Otitis externa, 380.1 |
| Eustachian tube dysfunction, 381.81 | Otitis media, acute with effusion, 381 |
| Foreign body, ear, 931 | Sinusitis, 473.9 |
| Furuncle, 680 | Temporomandibular joint (TMJ) |
| Immune deficiency, 279.3 | Tonsillitis, 463 |
| Impacted teeth, 520.6 | Lymphadenitis, 289.3 |
1. Otitis externa, otitis media with effusion (OME), sinusitis.
2. Mastoiditis, furuncle.
3. Foreign body, trauma.
4. Eustachian tube dysfunction.
5. Lymphadenitis.
6. Dental abscess, tonsillitis, impacted teeth.
7. Temporomandibular joint (TMJ) dysfunction.
8. Immune deficiency.
G. Treatment
(
Table 22-1
).
1. Pain management, especially during the first 24 hours, is a priority regardless of whether antimicrobial agents are prescribed. Acetaminophen and ibuprofen are the mainstays. Adequate dosage is important.
2. Observation involves deferring treatment for 48-72 hours in otherwise healthy children 6 months to 2 years of age with nonsevere illness at presentation
and
uncertain diagnosis and in children ages 2 years and older who present without severe symptoms
or
an uncertain diagnosis. There should also be a reliable parent or caregiver able to obtain medication if needed and adequate facilities for follow up and reevaluation.
3. Prescribe antibiotics with caution. More than 80% of cases resolve spontaneously.
4. For children age 2 years and older who appear well, discuss treatment options with parents which include:
a. Safety-net antibiotic prescription (SNAP) is a prescription for an appropriate antibiotic written to be filled within 5 days of the office visit. Parents are instructed not to fill the SNAP unless symptoms worsen at any time or symptoms do not improve during the waiting period of 48-72 hours. Instruct parents that child's condition may quickly progress to a more severe case and to call and make a return visit if this occurs.
b. 5-day course of high-dose amoxicillin (if no history of allergy).
5. Begin antimicrobial therapy
(Box 22-1)
if no improvement or condition has worsened within 24-72 hours.
6. Antibiotic therapy is indicated for symptomatic AOM, particularly in children younger than 2 years of age.
7. Prescribe amoxicillin (drug of choice) or ampicillin if causative organism unknown (most cases).
8. Initially prescribe amoxicillin 40-45 mg/kg per day for 5-7 days in uncomplicated cases in children younger than 2 years of age who do not attend daycare, have not taken antibiotics within the past 3 months, except in areas of high resistance. This dose may fail to eradicate DRSP.
9. If child attends daycare, has taken antibiotics recently, or has history of recent AOM, prescribe amoxicillin 80-90 mg/kg per day in 2 divided doses for 10 days.
10. Prescribe adequate dose for initial treatment of symptomatic children. If allergic to penicillin, treat with azithromycin (for children allergic to beta-lactam).
11. Not recommended in children younger than 6 months of age: 30 mg/kg (max 500 mg) once daily for 3 days; or 10 mg/kg (max 500 mg) once, then 5 mg/kg (max 250 mg) once daily for 4 days. Can also prescribe oral cephalosporins, macrolides, or trimethoprim-sulfamethoxazole (TMP-SMX; rates of resistance to pneumococci are high). Treat for 10 days.
12. Begin second-line therapy in cases of documented amoxicillin failure (e.g., persistent fever, ear pain, irritability, TM findings after 3 days of treatment of redness, bulging, or otorrhea). Drug must be active against beta-lactamase-producing strains of
H. influenzae
or
M. catarrhalis
, DRSP (e.g., oral amoxicillin-clavulanate [Augmentin]); give in higher doses of 80-90 mg/kg per day of amoxicillin component, clavulanate dose remains at 10 mg/kg per day or ceftriaxone (Rocephin) 50 mg/kg (max 1 g) IM once for severe infections and/or if compliance is concern.
13. If recurrence of acute symptoms after full course of amoxicillin, retreat with second-line antibiotic. First drug of choice is amoxicillin-clavulanate. Oral cephalosporins (except cefuroxime axetil) and macrolides do not provide adequate coverage against resistant strains of
S. pneumoniae.
14. Pain control (see beginning of section): warm compresses, an analgesic with antipyretic effects (e.g., acetaminophen or ibuprofen), and eardrops with benzocaine and antipyrine (Auralgan). Immediate treatment for pain is very important.
Box 22-1
Antibiotics Labeled for the Treatment of Acute Otitis Media
Penicillins
Amoxicillin (first-line therapy)
Other books
The Bazaar and Other Stories by ELIZABETH BOWEN
The Binding by Nicholas Wolff
Runaway Heiress by Melody Anne
Hot Seat by Simon Wood
For Camelot's Honor by Sarah Zettel
Dying to be Famous by Tanya Landman
Exiles in Arms: Night of the Necrotech by Werner, C. L.
Crimson Christmas by Oxford, Rain
A Bride for Kolovsky by Carol Marinelli