Pediatric Primary Care (77 page)

3. Subcutaneous nodule.
a. Small, hard nodules typically found on elbows, knees, wrists; also felt in occipital area, over vertebrae. Relatively rare finding in rheumatic fever.
4. Chorea.
a. Finding of abnormal, involuntary writhing, purposeless movements that extinguish with sleep.
b. Patients often have uncontrollable facial grimacing.
c. Often preceding emotional lability thought to be from CNS involvement.
d. Chorea is often late sign with latent period of 1-6 months.
5. Rash.
a. Erythema marginatum: typical rash of rheumatic fever; painless, does not itch. Spreads peripherally while central clearing, most common on trunk, limbs; face is usually spared.
6. Low-grade fever.
7. Painful joints without obvious joint inflammation.
E. Diagnostic tests.
1. Evidence of previous GABHS.
2. Modified Jones criteria to make diagnosis.
a. Major criteria:
• Carditis.
• Polyarthritis.
• Chorea.
• Erythema marginatum.
• Subcutaneous nodules.
b. Minor criteria:
• Arthralgia.
• Fever.
• Elevated acute-phase reactants (erythrocyte sedimentation rate, C-reactive protein, WBC count).
• Prolonged PR interval.
c. Diagnosis requires 2 major criteria, or 1 major and 2 minor criteria, and evidence of previous GABHS infection.
d. Electrocardiogram and echocardiogram for confirmed diagnoses.
F. Differential diagnosis.
| Congenital heart disease: 746.9 | Kawasaki disease. 446.1 |
| Infective carditis, 429.89 | Myocarditis, 429 |
| Juvenile rheumatoid arthritis, 714.3 |
1. Juvenile rheumatoid arthritis: small joints involved, swelling and deformities of joints, morning stiffness, no positive antistreptococcal antibody.
2. Kawasaki disease.
3. Congenital heart disease: murmur without associated symptoms of rheumatic fever.
4. Infective carditis or myocarditis: positive viral or bacterial cultures.
G. Treatment.
1. Prevention: appropriate diagnosis and treatment of streptococcal pharyngitis.
2. Referral to pediatrician or specialist if diagnosis suspected.
3. Antibiotics to eradicate streptococcal infection (primary prevention; see
Table 25-1
).
4. Bed rest until fever, symptoms resolve. With carditis, bed rest may be indicated for longer period of time.
5. Aspirin.
a. If no relief in arthritis with initiation of aspirin therapy, question diagnosis.
b. Steroids may be considered if no response to aspirin therapy and/or for those with moderate to severe carditis.
6. Secondary prevention (
Table 25-1
).
a. To prevent recurrence of rheumatic fever in susceptible individuals.
b. Antibiotics until 21 years of age and minimum of 5 years if no cardiac involvement.
c. Antibiotics until 21 years of age and minimum of 10 years if cardiac involvement but no residual cardiac disease.
d. Antibiotics until 40 years of age and minimum of 10 years if residual valve abnormalities; consider lifelong antibiotic prophylaxis.
H. Follow up.
1. With specialist.
2. Subacute bacterial endocarditis (SBE) prophylaxis if residual valve disease.
I. Complications.
| Valvular heart disease, 424.9 |
Table 25-1
Primary and Secondary Antibiotic Prophylaxis for Rheumatic Heart Disease
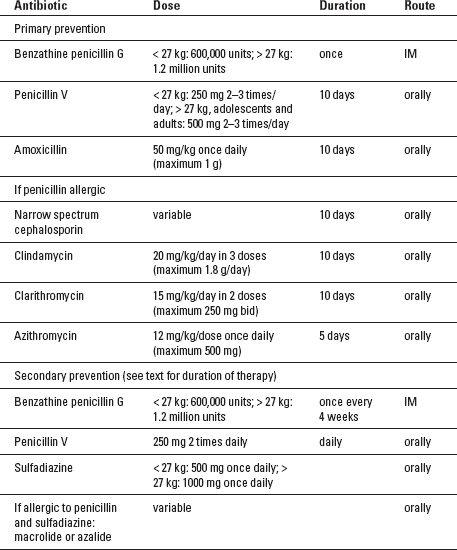
Source:
Adapted from: Gerber MA, Baltimore RS, Eaton CB, et al. Prevention of rheumatic fever and diagnosis and treatment of acute Streptococcal pharyngitis: a scientific statement from the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Committee of the Council on Cardiovascular Disease in the Young, the Interdisciplinary Council on Functional Genomics and Translational Biology and the Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics.
Circulation.
2009; 119(11):1541-1551.
1. Cardiac involvement.
a. Valvular heart disease.
2. Recurrence.
a. Increased risk of recurrence in susceptible hosts.
b. Cardiac damage is cumulative with each recurrence.
J. Education.
1. Nature of disease.
2. Recurrence risk.
3. Prompt diagnosis and treatment of Group A streptococcal pharyngitis.
4. Cumulative nature of cardiac damage with repeat episodes.
5. Secondary prevention.
a. Streptococcal infections do not have to be symptomatic to cause additional cardiac damage.
6. Importance of continued pediatric subspecialty follow up and transition to adult healthcare providers when appropriate.
7. SBE prophylaxis if indicated.
BIBLIOGRAPHY
Baker EJ. Non-rheumatic inflammatory disease of the heart. In: Anderson RH, Baker EJ, Penny DJ, et al., eds.
Paediatric cardiology.
2nd ed. Philadelphia, PA: Churchill Livingstone; 2010.
Coelho Mota CC, Demarchi Aiello V, Anderson RH. Rheumatic fever. In: Anderson RH, Baker EJ, Penny DJ, et al., eds.
Paediatric cardiology.
2nd ed. Philadelphia, PA: Churchill Livingstone; 2010.
Danford DA, McNamara DG. Innocent murmurs and heart sounds. In: Garson A, et al., eds.,
The science and practice of pediatric cardiology.
2nd ed. Baltimore: Williams & Wilkins; 1998.
Gerber MA, Baltimore RS, Eaton CB, et al. Prevention of rheumatic fever and diagnosis and treatment of acute Streptococcal pharyngitis: a scientific statement from the American Heart Association Rheumatic Fever, Endocarditis and Kawasaki Committee of the Council on Cardiovascular Disease in the Young, the Interdisciplinary Council on Functional Genomics and Translational Biology and the Interdisciplinary Council on Quality of Care and Outcomes Research: endorsed by the American Academy of Pediatrics.
Circulation.
2009;119(11):1541-1551.
National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation and treatment of high blood pressure in children and adolescents.
Pediatrics.
2004:555-576.
Takemoto CK, Hodding JH, Kraus DM.
Pediatric dosage handbook.16
th ed. Hudson, OH: Lexi-Comp; 2009.
Urbina E, Alpert B, Flynn J, et al. Ambulatory blood pressure monitoring in children and adolescents: recommendations for standard assessment: a scientific statement from the American Heart Association atherosclerosis, hypertension and obesity in youth committee of the Council on Cardiovascular Disease in the Young and the Council for High Blood Pressure Research.
Hypertension.
2008;52: 433-451.
CHAPTER 26
Gastrointestinal Disorders
Robin Shannon
I. ABDOMINAL PAIN, ACUTE
| Abdominal pain, acute, 789 | Mittelschmerz, 625.2 |
| Appendicitis, 541 | Ovarian cyst, 620.2 |
| Cholelithiasis, 574.2 | Pancreatitis, 577 |
| Colic, 789 | Pharyngitis, 462 |
| Constipation, 564 | Pelvic inflammatory disease (PID), 614.9 |
| Dysmenorrhea, 625.3 | Pneumonia, 486 |
| Ectopic pregnancy, 633.9 | Testicular torsion, 608.2 |
| Incarcerated hernia, 552.9 | Urinary tract infection, 599 |
| Intussusception, 560 | Viral gastroenteritis, 008.8 |
Other books
Til Death (Immortal Memories) by R. M. Webb
Baby Makes Five (A Multiple Birth Book 1) by Peters, Nicole
Sleepover Club Goes For Goal! by Fiona Cummings
Book of Nathan by Weeden, Curt, Marek, Richard
The Mobster And The Cowboy (A Cowboy Romance) by Mae Martini
Playing at Forever by Michelle Brewer
Daisy's Defining Day by Sandra V. Feder, Susan Mitchell
A Lost Lady by Willa Cather
The Man Who Came Too Much by Ellie Saxx
Treacherous by Barbara Taylor Bradford