Pediatric Primary Care (81 page)

3. Systemic illness: Are there signs of illness outside the GI tract?
4. Medication history: recent antibiotics? OTC diarrhea remedies? others?
5. Travel history.
6. Toxic ingestions?
7. Complete diet history: type, quantity of fluids; appetite; new/contaminated foods.
8. Urine output.
E. Physical findings.
1. Height, weight, temperature, vital signs.
2. Complete physical exam with attention to following:
a. Abdomen: assess bowel sounds, tenderness, organomegaly, masses, distention.
b. Rectal: Observe for stool around anus, erythema, fissures.
3. Assess hydration: activity level, irritability; degree of thirst; degree of dehydration
(
Table 26-1
)
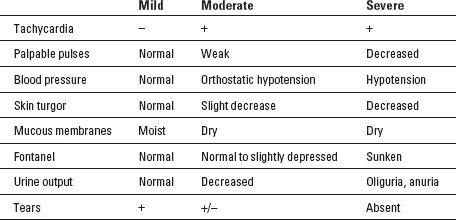
and signs/symptoms of dehydration
(
Table 26-2
).
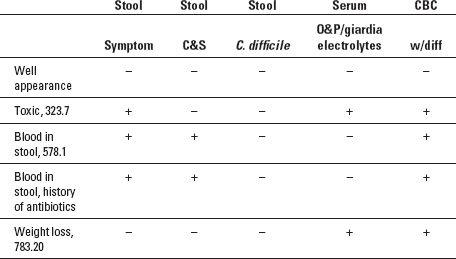
F. Diagnostic tests.
1. If patient appears nontoxic, mild/no dehydration: none; most episodes isonatremic.
2. Moderate to severe dehydration: serum electrolytes.
3. Test stool for occult blood
(
Table 26-3
).
Table 26-1
Assessment of Degree of Dehydration
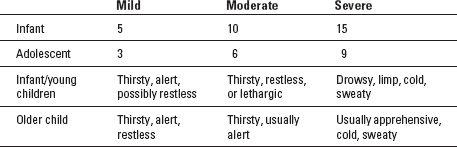
Table 26-2
Signs and Symptoms of Dehydration
4. When testing for
C. difficile
, ask for toxins A and B.
5. Not usually necessary to check for parasites unless diarrhea becomes chronic.
6. Test for rotavirus in stool if infant has moderate to severe symptoms.
7. Stool for
E. coli
0157:H7 is ordered separately.
8. Stool culture in febrile children with bloody diarrhea, check for
C. difficile
if recent antibiotic use.
Table 26-3
Diagnostic Testing for Diarrhea
G. Differential diagnosis.
| Adenovirus, 008.62 | Giardia, 007.1 |
| Allergic gastroenteritis, 558.3 | Norwalk, 008.63 |
| Antibiotic induced, 960.9 | Rotavirus, 008.61 |
| Bacterial, 008.5 | Salmonella, 003.9 |
| Clostridium difficile , 008.45 | Shigella, 004.9 |
| Cryptosporidium, 007.4 | Toxic ingestions, 558.2 |
| Diarrhea, 787.91 | Viral, 008.8 |
| Escherichia coli, 008 |
1. Viral: most common GI infectious cause: rotavirus, adenovirus, Norwalk.
2. Bacterial.
a. Salmonella: foodborne. Most resolve in 5-7 days without treatment. Fever, diarrhea +/- blood, abdominal cramping for 4-7 days.
b. Shigella: foodborne, usually during warmer months. Sudden high fever, abdominal cramps, nausea, vomiting, diarrhea with blood, mucus, pus. Usually self-limited. Dehydration common.
c.
E. coli
0157:H7: strain that produces toxin. Bloody diarrhea. Most common form of traveler's diarrhea, cause of most cases of hemolytic uremic syndrome (HUS).
e.
C. difficile:
found frequently in stool of children with antibiotic-associated diarrhea and in healthy infants, role as etiologic agent in these cases controversial. In pathologic cases, diarrhea can occur within days or up to 8 weeks after antibiotic use or any drugs that alter GI flora. Watery diarrhea, +/- blood. Fecal-oral route. Common in hospitals.
3. Parasitic.
a. Giardia: waterborne, foodborne. Diarrhea, bloating, abdominal cramping, nausea. Temporary lactase deficiency. Often self-limited. Outbreaks can occur in daycare and long-term care facilities.
b. Cryptosporidium: mild diarrhea, usually self-limited.
4. Dietary.
a. Increase in fluids with high osmotic load: fruit juices, sports drinks, or any sugared beverages can cause temporary osmotic diarrhea in otherwise healthy infant/child.
b. Introduction of new food: possible allergic response.
5. Antibiotic induced.
6. Toxic ingestions.
7. Systemic illness: may have history of upper respiratory infection (URI) or other illness.
H. Treatment.
1. Viral: self-limited, supportive care (see rehydration guidelines on p. 345).
2. Bacterial.
a. Salmonella: supportive.
b. Shigella: supportive, can be self-limited. Antimicrobial treatment for children in hospitals, daycare centers, institutions, and those with severe symptoms. Antibiotic resistance increasing: consult health department or MD for selection of appropriate antibiotic in your community.
c.
E. coli
0157:H7: supportive.
d.
C. difficile:
metronidazole (20-30 mg/kg/day divided tid for 10-14 days) oral.
3. Parasite.
a. Giardia: metronidazole (5-10 mg/kg/dose tid for 7-10 days) or nitazoxanide (Alinia) for children 1-11 years; 12-47 months: 5 mL (100 mg) bid for 3 days; 4-11years: 10 mL bid for 3 days; 12 and older 500 mg (1 tab) bid for 3 days, oral.
b. Cryptosporidium: supportive in immunocompetent patients; if therapy required: nitazoxanide.
4. Rehydration.
a. Mild dehydration: oral replacement solution 50 mL/kg (5 teaspoons/ pound) over 4 hours. Once repletion completed, ORS continued for ongoing diarrhea losses.
b. Moderate dehydration: oral replacement solution 100 mL/kg+replacement of stool losses over 4 hours, reassess hourly.
c. Severe dehydration: IV fluid: normal saline (0.9% saline); consult MD; transfer to tertiary care facility.
d. No dehydration: Continue to feed age-appropriate diet including milk.
5. Dietary.
a. Remove possible offending/allergenic foods.
b. No fruit juice, sports drinks, other sugared beverages.
c. Feed full diet: Restricting food deprives gut of nutrients needed for healing.
d. Continue to breast/formula feed, can alternate with oral replacement solution (ORS).
e. Eliminate dairy only if known giardia infection or if symptoms severe.
f. With dehydrated patient: refeed age-appropriate diet as soon as rehydrated.
6. Antidiarrheal medication/bismuth: avoid; not advised for children.
I. Follow up.
1. Telephone: Instruct parent to call and arrange for immediate clinic visit if not improving, new symptoms develop, signs of dehydration.
2. Return to clinic next day with mild-moderate dehydration.
3. Referral to MD or local ED for moderate-severe dehydration or lack of response to treatment.
Other books
Sold Out (Nick Woods Book 1) by Stan R. Mitchell
The Stager: A Novel by Susan Coll
When Darkness Falls by John Bodey
The Drazen World: Irrelevant (Kindle Worlds Novella) by Allyn Lesley
Stronger Than Sin by Caridad Pineiro
Dark Soul Silenced - Part Two by Simon Goodson
Mistress Mommy by Faulkner, Carolyn, Collier, Abby
The Maze (ATCOM) by Jennifer Lowery
Lie with Me by Stephanie Tyler