Resident Readiness General Surgery (14 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

COMPREHENSION QUESTIONS
1.
What does focal tenderness in the RUQ represent?
A. Acute cholecystitis
B. A high-riding appendix
C. Visceral inflammation
D. Peritoneal inflammation
2.
Do you need further imaging for a 19-year-old male patient with anorexia, nausea, vomiting, diarrhea, diffuse periumbilical abdominal pain, and a white count of 13?
A. Yes, because the Alvarado score is 7
B. Yes, because the Alvarado score is 4
C. No, because the Alvarado score is 7
D. No, because the Alvarado score is 4
3.
What
is not
on the differential for RLQ pain?
A. Meckel diverticulitis
B. Viral enteritis
C. Crohn disease
D. Ovarian cyst
E. PID
F. Ectopic pregnancy
G. Cancer
Answers
1.
D
. Focal abdominal tenderness represents focal peritoneal inflammation. While this could be secondary to either acute cholecystitis or a high-riding appendix, further testing would be needed. Visceral “tenderness,” as opposed to visceral pain, is not commonly encountered because visceral pain is not elicited by examination maneuvers—this principle underlies the phrase “pain out of proportion to exam.”
2.
D
. His Alvarado score is 4, which suggests he does not have acute appendicitis. It would be reasonable to watch the patient for progression versus resolution of his symptoms. To calculate the Alvarado score of 4, you score anorexia as 1 point, nausea and vomiting as 1 point, and a WBC >10,000 as 2 points.
3.
B
. Viral enteritis is not transmural and therefore does not cause localized peritoneal inflammation that would result in RLQ tenderness. The other items are worth memorizing for use when you are called to evaluate a patient with RLQ pain.
SUGGESTED READINGS
McGowan DR, Sims HM, Zia K, Uheba M, Shaikh IA. The value of biochemical markers in predicting a perforation in acute appendicitis.
ANZ J Surg
. 2013;83(1–2):79–83.
Pouget-Baudry Y, Mucci S, Eyssartier E, et al. The use of the Alvarado score in the management of right lower quadrant abdominal pain in the adult.
J Visc Surg
. 2010;147:e40–e44.
Ünlü C, De Castro SMM, Tuynman JB, Wüst AF, Steller EP, Van Wagensveld BA. Evaluating routine diagnostic imaging in acute appendicitis.
Int J Surg
. 2009;7(5):451–455.
 A 65-year-old Female in Severe Abdominal Pain
A 65-year-old Female in Severe Abdominal Pain
Aisha Shaheen, MD, MHA and Marie Crandall, MD, MPH
The emergency department house staff pages you to see Ms. Panosian, a 65-year-old female, who is complaining of severe, unremitting abdominal pain. Ms. Panosian tells you the pain is sharp and diffuse and began a couple of days ago. Eating makes her pain worse. Her vitals are:
Temperature 100.8
BP: 140/90
HR: 118
RR: 24
O
2
(%): 95% on RA
When you first see her, she appears very uncomfortable, but her vocalized complaints seem out of proportion to her physical exam findings. A digital rectal exam is positive for occult blood.
You initiate your diagnostic workup. Labs are notable for a WBC of 24,000 and a lactic acid of 4.4. Her ABG shows an early metabolic acidosis. While reviewing the chart, you noticed her EKG shows atrial fibrillation.
You go back to see the patient who tells you she is on chronic anticoagulation medication but ran out last week and has not refilled her prescription. You reexamine her and she now has generalized peritonitis.
You suspect ischemic bowel.
1.
Describe the physical findings associated with generalized peritonitis.
2.
Based on the presence of generalized peritonitis alone, would you say that Ms. Panosian has early or late ischemic bowel?
3.
What is the most appropriate next step?
4.
List 3 other surgical causes of generalized peritonitis.
5.
List 3 nonsurgical causes of generalized peritonitis.
6.
You inform your senior resident about Ms. Panosian and she instructs you to “optimize” the patient for the operating room and begin empiric antibiotic coverage. What organisms should be covered?
ACUTE ABDOMEN
Answers
1.
Generalized peritonitis is inflammation of the parietal peritoneum. It can result from any inflammatory or infectious disease process that occurs in the abdomen including rupture of a hollow viscus and spillage of gastrointestinal contents, bile, blood, or bacteria.
As with all processes that involve the peritoneum, the pain in generalized peritonitis is constant and sharp. It is also associated with reflexive contraction of the abdominal wall and, on physical exam, “board-like” rigidity. Even lightly tapping on the abdominal wall will usually elicit pain. The patient will sometimes report that, on the trip to the hospital, every bump in the road was excruciating.
2.
Ischemic bowel initially results in visceral pain—the visceral afferents of the bowel are exquisitely sensitive to ischemia. In this early phase there is no inflammation of the peritoneum and therefore no somatic pain or any signs of peritonitis. The lack of peritonitis explains the classic teaching that patients with early ischemic bowel have “pain out of proportion to physical exam.”
If the ischemia is not reversed, however, transmural inflammation and eventually necrosis will ensue. Even if the bowel doesn’t perforate, the inflammation irritates the peritoneum and therefore causes peritonitis localized to the area of the abdomen in which the bowel is ischemic. When the bowel perforates, bowel contents are spilled into the abdominal cavity, leading to generalized peritonitis. Given the progression of Ms. Panosian’s exam, she has most likely perforated and this is therefore relatively “late” ischemic bowel.
3.
Generalized peritonitis often represents an “acute” abdomen, meaning urgent surgical intervention is mandatory. As such, when an intern or junior level resident is consulted on a patient with this finding, the information should be relayed to a senior resident in an expeditious manner. This is best done by performing a quick but thorough history and physical exam and then letting the senior resident know you have a patient who may require emergent surgery. In the meantime, standard labs should be ordered (at a minimum CBC, chemistries [BMP], venous blood gas [VBG], and coags).
4.
A variety of disease processes, both surgical and nonsurgical, can cause generalized peritonitis. Surgical causes include the rupture of any hollow viscus (eg, ruptured appendicitis, perforated peptic ulcer, or perforated diverticulitis) as well as any process that results in intraperitoneal blood (eg, traumatic hemorrhage). Less common surgical causes include ruptured ectopic pregnancy or a large segment of infarcted and inflamed bowel.
5.
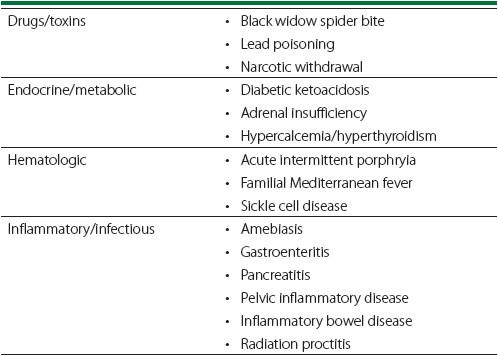
Nonsurgical causes of generalized peritonitis can be divided into 4 major categories: drugs/toxins, endocrine/metabolic, hematologic, and inflammatory/infectious (see
Table 11-1
).
Table 11-1.
Nonsurgical Causes of Generalized Peritonitis
6.
Once generalized peritonitis is diagnosed and the underlying cause is identified as being surgical in nature, the patient should be expeditiously prepared for the operating room. This preparation involves correction of any electrolyte disturbances, IV hydration, and appropriate antibiotic coverage. The antibiotic regiment should be started immediately on diagnosis and should initially be broad enough to cover the most likely causative agents. For the gastrointestinal tract the major involved pathogens are likely to be gram-negative enteric organisms (
E coli
,
Klebsiella
) and anaerobes (
B. fragilis
). Appropriate coverage can be obtained with the combination therapy of a third- or fourth-generation cephalosporin (ceftriaxone, cefepime) or a fluoroquinolone (ciprofloxacin or levofloxacin) + metronidazole (Flagyl). Single-agent therapy with a β-lactam (Zosyn) or carbapenem (imipenem-cilastatin) is another alternative. After culture results have been obtained, the antibiotic regimen can be tailored to cover the organisms identified.
TIPS TO REMEMBER
Generalized peritonitis, or an “acute” abdomen, mandates urgent surgical evaluation.
A variety of surgical diseases including ischemia, infection, obstruction, and perforation can result in generalized peritonitis.
Key exam findings for generalized peritonitis include sharp pain, abdominal distension, and peritoneal signs such as guarding, rigidity, and rebound tenderness.