Resident Readiness General Surgery (52 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

 A 70-year-old Postoperative Colectomy Patient Who Is Not Putting Out Much Urine
A 70-year-old Postoperative Colectomy Patient Who Is Not Putting Out Much Urine
Brian C. George, MD and Alden H. Harken, MD
“Doctor, your postop colectomy patient isn’t putting out much urine.”
Mr. O’Flaherty is a 70-year-old gentleman who is two hours post left colectomy. His vitals are: BP 110/70, HR 110 (regular), respiration 18, and temperature 37.5°C. In the last hour he has made 15 mL of urine.
1.
List at least three clinical indicators of adequate peripheral perfusion.
2.
What does a spot urine sodium of 12 mEq/L in a postoperative patient mean?
3.
What does anuria usually represent?
4.
In the vignette presented above, should you give the patient some furosemide to fix his oliguria?
POSTOPERATIVE OLIGURIA
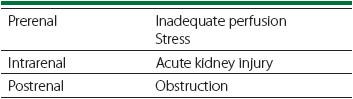
There are multiple possible causes of oliguria in the postoperative patient, although inadequate renal perfusion is the most common. Stress, acute kidney injury, and obstruction are other common causes (see
Table 40-1
). We will address each of these in turn.
Table 40-1.
The Most Common Causes of Oliguria
Answers
1.
As surgeons, we use multiple reassuring indicators of adequate cardiac output and hemodynamic stability, which include:
Invasive indicators
:
A. Blood lactic acid
B. Blood metabolic acid (pH >7.35 without respiratory compensation; so, PaCO
2
>35 mm Hg)
C. Mixed venous O
2
sat >65% (requires a central venous or pulmonary artery catheter)
Less invasive indicators:
A. Stable BP (relative to preoperative)
B. Stable heart rate
C. Comfortable respiratory rate (when you are sick, or running up stairs, you breathe faster)
D. Big toe temperature (short of sepsis, if your big toe is warm, you’re doing OK)
E. Urine output
The focus of this chapter is the last item on this list: urine output. Because the kidneys are exquisitely sensitive to changes in cardiac output, oliguria can indicate that your patient has compromised renal perfusion—usually but not always due to hypovolemia. Note that using urine output as a measure of end-organ perfusion is very similar to using goal-directed therapy (GDT) principles as described in the chapter on Shock.
Hypovolemia in the acute postoperative period is usually due to one of two causes. Most commonly it is the result of so-called third spacing, where leakage of plasma into the surgical field (and beyond!) results in depleted intravascular volume. However, hypovolemia can also be due to hemorrhage, which must always be in the back of your mind.
When treating an acutely postoperative patient who you believe is oliguric due to hypovolemia, a standard approach is to give a 500 mL to 1 L bolus of crystalloid. If the patient does not respond as expected within 30 minutes, then you should begin looking more carefully for other potential causes of inadequate cardiac output. This should include a CBC to evaluate for hemorrhage as well as a spot urine sodium (see below).
While hypovolemia is the usual focus of surgeons, it is important to remember that oliguria is also a normal response to stress. Stretch receptors in the left atrium, sensitive to low pressure, signal release of antidiuretic hormone (ADH or vasopressin) from the pituitary. Volume depletion, positive pressure ventilation, pain, nausea, and many other types of “stress” all provoke release of both ADH and mineralocorticoids (aldosterone). So, surgical stress promotes volume retention directly (via ADH) and less directly by renal retention of sodium (via aldosterone).
2.
While oliguria may indicate reduced renal perfusion or increased ADH and aldosterone, it can also be because your patient has sick kidneys. In order to distinguish between those alternatives, you obtain a urine sodium. If the
urine sodium is less than 10 to 15 mEq/L, your patient’s kidneys are working flat out (ie, beautifully) in response to stress. You can infuse some crystalloid and urine volume will increase. If, however, the urine sodium is elevated (say, 40–50 mEq/L), then your patient’s kidneys are sick. Now, you have bigger trouble because there are no direct pharmacological agents that protect renal health. Do everything that you can to preserve kidney perfusion (be sure to still optimize cardiac output) and meticulously check for any nephrotoxic agents that your patient may inadvertently be receiving.
To sort out oliguria, you can calculate a fractional excretion of sodium (FENA). The FENA represents the percentage of sodium filtered by the kidneys that is excreted in urine. A kidney is a high-volume system, and in a healthy adult surgical resident, after dilution in the loop of Henle, approximately 20 L of hypotonic fluid reaches the collecting system each day. Thus, in the total absence of ADH (diabetes insipidus) a patient will put out 20 L of urine daily. The urine sodium depends on both renal water reabsorption and the health of the tubular sodium reabsorptive function. Mathematically, the formula looks like:
FENA = 100 × (urinary Na over plasma NA)
× (plasma creatinine over urinary creatinine)
FENA <1% indicates hypovolemia.
FENA >3% indicates sick kidneys.
FENA between 1% and 3% indicates “I’m not sure.”
Now, you can make these calculations even more inscrutable, but for all practical purposes, when you are confronted with an oliguric patient, you can usually just get a urine sodium.
A. If it’s less than 15 mEq/L, try some crystalloid.
B. If it’s higher than 40 to 50 mEq/L, you need to worry.
3.
Whenever you are called about a patient with oliguria who has a Foley in place, you must convince yourself that the catheter is patent. Bladder distension and anuria should prompt you to have the Foley flushed. New anuria is highly specific for catheter obstruction—even sick or hypoperfused kidneys usually make a little urine.
4.
The use of furosemide (Lasix) in an oliguric patient should not be initiated until it has been determined that the cause of the oliguria is not a lack of renal perfusion. In that case, diuresis reduces the circulating volume that in turn decreases preload and cardiac output, thereby worsening the situation. If, on the other hand, the cause of the oliguria is intrinsic, then one can argue that high-output renal failure is easier to manage than low-output renal compromise. The one circumstance in which furosemide is clearly indicated for oliguria is when a patient is hypoperfusing his or her kidneys due to congestive heart failure—in this case, diuresis can be predicted to improve cardiac output.
TIPS TO REMEMBER
We use urine output as a “composite” indicator of a patient’s hemodynamic stability.
Oliguria is a normal response to stress.
A stressed patient retains volume directly (via ADH) or less directly by renal retention of sodium (via aldosterone).
A spot urine sodium less than 15 mEq/L means your patient’s kidneys are healthy; give crystalloid.
A spot urine sodium greater than 40 to 50 mEq/L means your patient’s kidneys are sick; optimize renal perfusion and search for any nephrotoxic drugs your patient might be receiving.