Resident Readiness General Surgery (51 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

BOOK: Resident Readiness General Surgery
11.09Mb size Format: txt, pdf, ePub
Bulk laxatives
—these work by colonic distention, triggering peristalsis:
1.
Psyllium (Metamucil) 1 tbsp BID—hygroscopic husks absorb water and become mucilaginous (jello-like).
2.
Methylcellulose (Citrucel).
3.
Calcium polycarbophil (Fibercon).
4.
Guar gum (Benefiber).
Osmotic laxatives
—as a class, these act as hyperosmolar agents, drawing water into the lumen of the intestine as well as stimulating colonic activity via cholecystokinin:
1.
Lactulose/70% sorbitol—poorly absorbed sugars:
A. Sorbitol is sweeter than sucrose with ~1/3 fewer calories.
B. Sorbitol is significantly less expensive than lactulose.
C. Lactulose converts ammonia to nonabsorbable ammonium ion.
2.
Magnesium salts:
A. Magnesium ions stimulate the activity of nitric oxide (NO) synthase and increase levels of the proinflammatory mediator platelet activating factor (PAF) in the GI tract.
B. NO may stimulate intestinal secretion via prostaglandin- and cyclic GMP–dependent mechanisms while PAF produces significant stimulation of colonic secretion and gastrointestinal motility.
C. Can cause hypermagnesemia and hypocalcemia.
3.
Sodium salts:
A. Phospho-soda (OsmoPrep).
B. Fleet Enema (sodium phosphate)—can cause hyperphosphatemia and hypocalcemia.
4.
Polyethylene glycol 3350 (Miralax):
A. Seventeen grams in 8 oz liquid once or twice daily.
B. Safe in renal failure.
Stimulant laxatives
—these alter water and electrolyte transport in the colon and increase colonic motility by causing low-grade inflammation in the colon through activation of prostaglandin/cyclic AMP and NO/cyclic GMP pathways:
1.
Bisacodyl (Dulcolax)—diphenylmethanes inhibit water absorption in the small intestine and act via direct parasympathetic stimulation of mucosal sensory nerves, increasing peristaltic contractions.
2.
Senna
extracts (Ex-lax, Senokot)—anthraquinones act on enteric neurons and intestinal muscle to produce giant migrating colonic contractions in addition to stimulating water and electrolyte secretion.
3.
Importantly, perforation and obstruction must be ruled out prior to giving stimulant laxatives!
Emollient laxatives
—these act as stool softeners and are more effective in conjunction with stimulant laxatives:
1.
Docusate sodium (Colace).
2.
Glycerin suppository—exerts a hyperosmotic effect drawing water into the rectum; allows water and fat to penetrate the fecal mass.
3.
Mineral oil:
A. Poor oral choice.
B. Aspiration causes lipoid pneumonia; depletes fat-soluble vitamins.
C. Lubricates stool when given as an enema.
4.
Soapsuds enema—should not be used due to irritation of the colonic mucosa and risk for hemorrhagic colitis.
Novel agents:
1.
Methylnaltrexone (Relistor):
A. Mu-opioid antagonist that does not cross the blood–brain barrier.
B. Indicated only for opioid-induced constipation.
C. Injectable.
D. Expensive.
2.
Lubiprostone (Amitiza)—bicyclic fatty acid, activates type II chloride channels in the apical membrane of the GI epithelium resulting in increased secretion of chloride and subsequently water:
A. Contraindicated in pregnancy.
4.
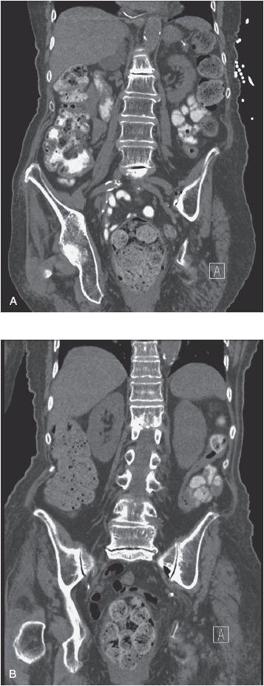
Fecal impaction: a firm mass of immovable stool in the rectum or distal colon; relatively common in the elderly, especially the bed-bound nursing home population. In one study, fecal impaction was found to be responsible for 55% of cases of diarrhea in hospitalized elderly patients (see
Figure 39-2
A and B).
Figure 39-2.
(
A
and
B
) CT images of a patient with fecal impaction and a hx of stercoral colitis.
Steps in manual disimpaction:
1.
Consider analgesia and/or sedation.
2.
Position the patient in the lateral decubitus or dorsal lithotomy position.
3.
Soften impaction with mineral oil enema or glycerin suppository.
4.
Lubricate impaction.
5.
Break up impaction with scissoring motion of 2 fingers.
6.
Can follow with tap water or sodium phosphate enema.
7.
Start regular bowel regimen to prevent recurrence.
Impaction of stool may be prevented by following a high-fiber, fluid-rich diet; getting regular exercise; limiting intake of constipating drugs; routinely using stool softeners or laxatives; and learning biofeedback and habit training.
TIPS TO REMEMBER
More than 50% of patients taking narcotic pain relievers will develop dose-dependent constipation. A reasonable prophylactic regimen includes a combination of a bulking agent and a stimulant laxative.
Plain films of the abdomen can reveal impacted stool, dilated proximal loops of bowel, air–fluid levels, and the presence of free intra-abdominal air (in the case of perforation). The normal maximal diameter of the colon is 6 cm and that of the rectum is 4 cm.
Manual disimpaction involves softening, lubricating, and fragmenting the hardened stool.
COMPREHENSION QUESTIONS
1.
Which of the following is contraindicated in patients with renal failure?
A. Psyllium
B. Sodium phosphate (Fleet Enema)
C. Sorbitol
D. Polyethylene glycol
2.
Which of the following is not associated with constipation?
A. Verapamil
B. Furosemide
C. Loperamide
D. Metronidazole
Answers
1.
B
. Sodium phosphate can cause hyperphosphatemia. In high-risk patients, it can cause an acute nephropathy.
2.
D
. Although a treatment for diarrhea caused by
C. difficile
colitis, metronidazole is more commonly implicated in antibiotic-associated diarrhea itself.
Other books
Blood and Daring by John Boyko
Too Grand for Words (BookStrand Publishing Romance) by Natasza Waters
Victoria's Demon Lover by Bess, Alia
Imposter by Antony John
Livvie Owen Lived Here by Sarah Dooley
Papeles en el viento by Eduardo Sacheri
The Master Falconer by Box, C. J.
Lusam: The Dragon Mage Wars Book Two by Cadman, Dean
Tails of Spring Break by Anne Warren Smith
The End of the World as We Know It by Robert Goolrick