The Guide to Getting It On (124 page)
Read The Guide to Getting It On Online
Authors: Paul Joannides
Tags: #Self-Help, #Sexual Instruction, #Sexuality

IUDs—A Great Choice for Teens,Young Women, and Women of All Childbearing Ages
IUDs are one of the most widely used contraceptives in the world. In North America, they have the highest user satisfaction ratings among all methods of reversible birth control, including the pill, patch, ring, shot and condom. IUD’s are also the most effective method of reversible birth control.
It doesn’t matter if you are teenager and have never been pregnant and if you enjoy having sex with more than one guy—an IUD should work very well for you. Like most birth control methods besides condoms, an IUD won’t prevent you from getting a sexually transmitted infection, but it won’t make you more likely to get one, either. If you get a sexually transmitted infection, it would be your fault, not on the IUD. And most sexually transmitted infections can be treated without having to take out your IUD.
Today’s IUDs are incredibly safe. More than 20% of female OB/GYNs personally use IUDs as their method of birth control. Almost 20% of women in Asia use IUDs, and 15% of women in Europe.
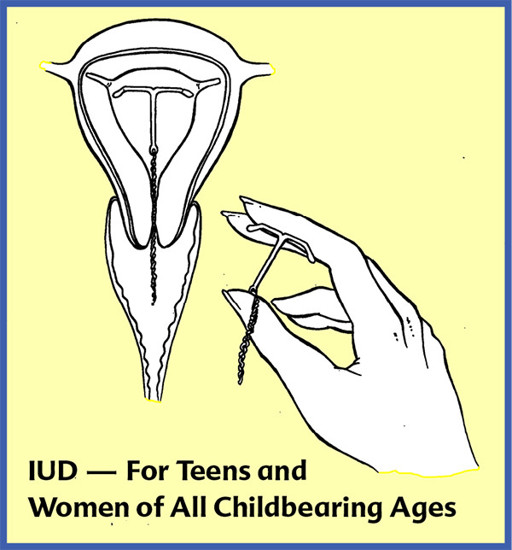
IUD stands for “intrauterine device.” It is a small T-shaped device that is placed in the uterus to prevent pregnancy. There are two kinds, one that has hormones (Mirena) and one that releases copper ions instead (ParaGard). The hormone-releasing Mirena can stay in for up to 7 years. It is better for women who have crampy or heavy periods, as it helps lighten bleeding or it can eliminate periods altogether. The Paragard IUD is great for women who want a regular period and no hormones. It can last up to ten years.
Both the copper IUD and Mirena protect against endometrial cancer. It also appears they help prevent ectopic pregnancies, and the Mirena IUD helps shrink uterine fibroids and reduces the symptoms of endometriosis.
Women who are wearing IUDs can become pregnant within a week of having the IUD taken out. IUDs only impact fertility when they are in a woman’s body. Studies are showing that a woman is more likely to conceive sooner after having an IUD removed than after she stops taking the pill.
How IUDs Work: the copper in the Paragard IUD keeps the sperm from maturing once they enter the cervix. The progestin in the Mirena IUD acts the same as progestin does in progestin-only birth control pills, or the Implanon implant and Depo shot. IUDs do not work by causing a low grade infection in the uterus. That is one of the unfortunate myths that some people have about IUDs.
The ParaGard (copper IUD) might be the best birth control choice for most female athletes. It is highly effective, hassle free, and doesn’t put out hormones that might result in water retention or soreness. The Mirena IUD might be the best control for women who have Category 5 periods with heavy flow. A lot of women find that it stops their periods in 6 to 12 months.
If an IUD is going to be expelled, the time when that is most likely to occur would be during the first menstrual cycle. The chances of this happening are low, and after your first period it is very unlikely that a uterus will send an IUD packing. Once it is in place, an IUD should not cause discomfort. A woman shouldn’t know it’s there. The only part of an IUD that can be felt is two very thin nylon strings that hang down from the IUD. If a man is able to feel the strings during intercourse, a healthcare provider can easily snip them to be shorter.
Most women find there to be little or no pain when the IUD is inserted. Some find the pain to be moderate but manageable, and a small number of women find the pain to be terrible. If you are concerned, discuss this with your healthcare provider.
In our survey of gynecologists who insert a large number of IUDs, many felt ibuprophen an hour before insertion works well for pain management, others suggest tramadol, diazepam or misopristol as long as the woman has a ride home. All agreed that satisfaction with the IUD is high among their patients. They felt it was a great choice for younger women.
The one thing you need to be sure of is that your healthcare provider has substantial experience installing IUDs. With experience comes mastery, so ask how often the person puts in IUDs.
The initial cost of an IUD can be high, but is usually much cheaper over the lifetime of the IUD than any other form of birth control. Fortunately, an IUD is free if you fall under the umbrella of the Affordable Healthcare Act. If your insurance doesn’t cover the cost of an IUD and money is a concern, be sure to shop around. Also check with your local Planned Parenthood.
An unfortunate myth about IUDs is they are not safe. This comes from what happened in the early 1970s with an IUD called the Dalkon Shield. The reason why the Dalkon Shield caused infections was because of the material used in the tailstring as opposed to the IUD itself. The material in the tail string allowed bacteria from the vagina to wick into the cervix. That kind of material is no longer used and the FDA now regulates IUDs, which it didn’t in the 1970s. Even though the manufacturer knew about the problem from almost the beginning, they hushed it up and ramped up their marketing efforts to get more women to use that ill-fated IUD.
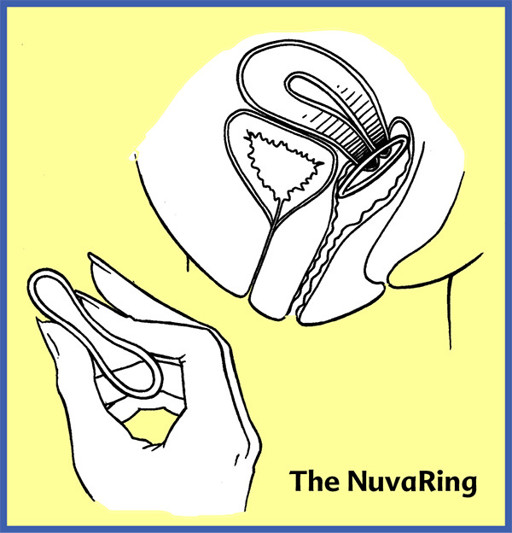
The NuvaRing
The NuvaRing is a 2” diameter plastic ring with hormones in it. A woman puts it in her vagina on day one of her menstrual cycle and takes it out on day 21. The NuvaRing eliminates the need to take a pill every day, to get an injection or to wear a patch. Aside from the Mirena IUD, a woman will be hard pressed to find a hormonal method of birth control that is more user-friendly than the NuvaRing.
Because the hormones absorb directly into the blood stream, the dosage of hormones a woman receives from the NuvaRing may be lower than what is in most birth-control pills. However, it still has the same side effect profile as birth control pills and other hormonal methods.
The NuvaRing is one of the few hormonal methods of birth control associated with greater vaginal lubrication rather than less, although some women finds it dries them out. Also, some women report leaving the Nuva Ring in for an entire month for period suppression, but please speak to your healthcare provider before trying this.
The NuvaRing sits in the same place as a diaphragm, only a woman doesn’t need to worry if it’s exactly in place because it isn’t a barrier. It is fine if it moves around. One size fits all. The muscles in the vagina hold it in place, and most women can’t feel it. If for some reason a woman’s partner can feel the NuvaRing during intercourse, a woman can take the NuvaRing out for up to three hours at a time. If her partner can’t finish doing his business in three hours, she should consider sending him to the bathroom with a jar of hand cream while she puts her NuvaRing back in.
The Pill
The pill is a hormonal method of birth control that works by stopping the eggs from leaving the ovary. As a result, ovulation does not occur. They also work by causing the cervical mucus to become thicker, which inhibits the effectiveness of sperm. Women take the pills for 21 or 28 days, although a lot of pill packages come with 7 dummy or reminder pills that have no hormones in them. A woman takes the reminder pills from days 21 to 28 to allow her to have a period. This creates a 28-day cycle.
Many women find the pill to be a great birth control, while others find the side effects to be undesirable or intolerable. The side effects include a decrease in sex drive. (For a discussion of this, see Chapter 59:
The Pill and Your Sex Drive.)
There are more than fifty different kinds of birth-control pills and it can be an art to get an optimal match between patient and pill. The clinical skill of a healthcare provider and their willingness to inquire and experiment are important elements of the process. If the first brand a woman takes does not fit with her body chemistry, there are other combinations and forms of hormonal birth control. Unfortunately, not many women are aware of their choices.
As for the pill’s safety, a long term study that has followed thousands of former pill-taking women for forty years. These women had taken the pill for at least four years. The women who had taken the pill are living longer than controls who didn’t take the pill. This isn’t to say that bad things can’t happen, but they tend to be rare and the risks of taking the pill are not nearly as great as the risks of being pregnant.
If a woman is considering a hormonal method of birth control, the first thing to consider is what she wants it to do for her. Is it just for pregnancy prevention? Or is it also to help tame harsh periods or to eliminate periods altogether? A woman should talk to her healthcare provider about the advantages, disadvantages and side effects of the different hormonal methods.
A woman also needs to be honest with herself regarding her ability to remember to take a pill each day. If the mere thought of this would cause the collective jaws of her family and friends to drop, she should consider an IUD, the NuvaRing, an implant or the Depo-Provera shot instead. All it takes is one missed pill for the effectiveness of the pill to go down. Also, the effectiveness of the pill can be impacted by antibiotics and other prescriptions a woman might be using. Whenever a woman who is using hormonal methods of birth control is given a prescription for another drug, she should be sure to ask if it will impact the effectiveness of the birth control pill.
Most birth control pills contain a combination of estrogen and progestin. A woman usually takes an active pill with hormones in it each day for 21 straight days.
Progestin-Only Pills, or POPs:
Progestin-only pills only contain progestins. In fact, the original birth-control pill was made of progestins only. Progestin-only pills are called POPs or mini-pills. They are used by women who cannot take estrogen, including those who smoke and are older than 35, as well as women who have heart disease, high blood pressure or are at risk for blood clotting. They can be helpful for women who have heavy bleeding or cramping during their periods. POPs are often better than estrogen-containing methods for women who get migraines or focal neurological deficit. They are also used by nursing mothers and women with sickle cell anemia.