The Ins and Outs of Gay Sex (15 page)
Read The Ins and Outs of Gay Sex Online
Authors: Stephen E. Goldstone

Typically, Condyloma acuminatum appears on your anogenital region, including your penis, anus, scrotum, pubic region, inner thighs, buttocks, and anal canal.
The time between the virus landing on your body and the appearance of your wart is very variable, lasting anywhere from six weeks to eight months and occasionally as long as years.
Most doctors believe the average incubation period is about three months, but keep in mind that the virus doesn’t always grow into a wart.
This becomes a major issue for gay men in monogamous relationships when partners automatically assume that the presence of warts on one means cheating.
Well, don’t assume anything.
Just because warts turned up now doesn’t mean that you just caught the virus.
It could have been hanging out on your body for years, put there by one of your
previous
boyfriends.
Even after warts have been completely destroyed, the virus may remain dormant in your cells.
Some doctors believe you never get rid of HPV, and any recurrence represents a reactivation of virus you already had, not a new infection.
And before you accuse your partner of cheating, look in the mirror.
You could have brought the virus to him!
Just because a wart didn’t grow on you doesn’t mean you’re free of HPV.
Unlike the uniform appearance of molluscum, condyloma
can all look very different.
They vary from a whitish color to a shade lighter (hypopigmented) or darker (hyperpigmented) than your normal skin.
(See
Figure 4.
3
.
) Most are raised and resemble tiny bunches of cauliflower, while others appear more like dark skin blemishes.
If you find one wart, you can bet you have others in various stages of development.
I have seen warts neglected for so long that they cover the man’s entire buttocks.
At this stage they usually have a foul order and ooze a purulent (infected) fluid.
I am always stunned when I ask a patient why he didn’t come in sooner and he answers, “But I just noticed this.”
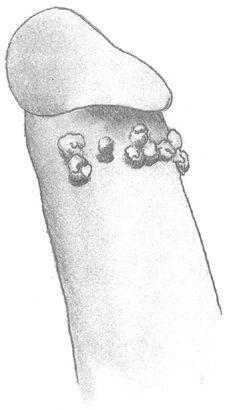
Figure 4.
3:
Condyloma Acuminatum
Although warts often cause itching, the most common first symptom is the wart itself.
It gradually increases in size and others appear.
If you have anal warts, rectal bleeding and pain after bowel movements and anal sex are other common complaints.
Occasionally an anal wart creates a painful fissure that fails to heal without surgery.
Warts on your penis probably won’t cause any symptoms at all.
Although unsightly if they grow large, they aren’t painful and rarely bleed.
Penile warts can spread down your urethra (the tube that carries urine through your penis) and cause bleeding or burning with urination.
So you think you’ve got them; now what do you do?
See your physician immediately.
A diagnosis often can be made visually, and biopsy is seldom necessary.
Don’t be startled if your doctor wraps a gauze soaked in vinegar around your penis or places it against your anus.
Vinegar (acetic acid) turns warts white and helps your physician identify them.
Which brings me to another important point:
All bumps on your penis or anus are not warts.
Hair follicles are often raised.
If you suspect a wart and routinely shave your genitals, stop, because shaving inflames hair follicles and makes the diagnosis more difficult.
Skin tags are also commonly found in this area but bear no relation to warts.
They do not need to be removed unless you find them unsightly.
So relax and let your doctor put on the acetic acid.
It won’t hurt, the acid is very dilute.
If you have warts around your anus, be sure your physician inserts a small lighted scope (anoscope) into your anus and looks on the inside as well.
Don’t be frightened, the scope is less than six inches long and not very thick.
Discomfort is minimal and the exam takes less than a minute.
If your doctor says it isn’t necessary or can’t perform this simple test (many dermatologists and internists don’t have the capability in their offices), find one who will.
What is visible on the outside of your anus is usually just the tip of
the iceberg; you probably have many more warts on the inside.
If your doctor only treats your external warts, they will continue to recur.
Each time you move your bowels you push human papillomavirus out with your feces and reinfect your skin.
I have had patients refuse anoscopy saying “You don’t have to look inside because nothing has ever gone up there.”
Wrong!
Each time you wipe after a bowel movement, fingers and toilet paper gently probe your opening, and virus can easily be pushed inside.
Other patients argue that they couldn’t possibly have warts because they’ve checked their partners thoroughly.
Unfortunately, just because you don’t see a wart doesn’t mean he isn’t carrying the virus.
Warts are five to ten times more common in the anal canals of gay men than on their penises.
No one knows what stimulates a virus to blossom into a wart, but we do know that it grows better in the moist anal area than on a penis.
Consequently, virus from your partner’s penis where a wart
doesn’t
grow gets transmitted to your anal area where it does grow.
So you have warts; now what do you do?
Have them removed.
If you don’t, they will continue to grow, spread to others, and possibly change to cancers.
Do not treat warts yourself with over-the-counter preparations meant for hands!
In case you haven’t noticed, your penis is not your finger.
Venereal warts are more numerous than typical hand warts—especially in your anus—and you cannot do a thorough job.
Putting caustic lotions meant for hands into your anus can be very dangerous.
I know you want to tell me that you’ve heard of cases of warts disappearing on their own.
That’s true; there are
isolated
reports in the medical literature of spontaneous regression of condyloma, but the incidence is rare.
All I can say is:
“Don’t count on it.
See your doctor.”
Treatments available for condyloma through your doctor
are numerous and varied.
Which one is best?
The only way to answer this frequently asked question is to repeat what a physician friend of mine always says:
“If one treatment was unequivocally better than the others there wouldn’t be so many alternatives available.”
When a report in the medical literature proclaims one treatment as best, it isn’t long before another contradicts those same results.
The following are the most common procedures and medications available through your physician.
Familiarize yourself with them so you can discuss the pros and cons of each before settling on a course of action.
TOPICAL AGENTS
Topical medications have long been the mainstay of condyloma therapy.
In essence, a caustic cream or liquid applied directly to a wart erodes it layer by layer.
Podocon-25 (podophyllin), manufactured from a plant resin, is the most common medication in this class and was first used to treat condyloma in the 1940s.
Your doctor dabs it on your warts, and you wash it off twelve hours later.
Podophyllin will burn surrounding skin unless applied carefully and requires reapplication every one to two weeks until the wart completely disappears.
Scarring rarely occurs.
Trichloroacetic acid is another common topical agent many doctors use.
Like podophyllin, it’s applied weekly until your wart disappears but has the added advantage of not needing to be washed off.
Both agents irritate normal skin if not used carefully.
A slight burning sensation after application is common but quickly passes.
While small warts may go away with just one treatment, larger warts can require repeated applications over weeks or even months.
Podofilox (Condylox) is available by prescription and, unlike the other two medications, it is designed for home use.
Apply it to external warts only, twice daily for three days, followed by a four-day rest.
Repeat the cycle each
week until your warts disappear, but be sure your doctor monitors your progress.
Topical medications are best used on penile warts, which are usually isolated and easily identified.
Recurrence is rare when treatment continues until the wart completely disappears.
If penile warts keep coming back after
complete
resolution, see a urologist.
You may have warts inside your urethra that keep seeding the outside skin.
Although some physicians recommend caustic topical agents for perianal warts, I usually advise against it.
Perianal warts in gay men, as mentioned earlier, are usually just the tip of the iceberg; the most advanced lesions are inside the anal canal.
Although these medications can cure warts outside your anus, don’t expect the cure to last.
Untreated warts inside your anal canal will continually reinfect your perianal skin.
Some doctors think that just swabbing your anal canal blindly with a topical agent is enough to destroy internal condyloma.
No such luck.
Your rectal lining is folded like a pie crust, so each fold must be spread open to expose hidden warts.
Random application inside your anus and rectum misses some warts while burning completely normal areas.
Topical agents applied within your anus and rectum also can cause severe pain and a bloody rectal discharge.
What do you do if after a thorough internal examination your doctor is positive all your warts are on the outside?
Try topical agents, but watch closely to be sure your warts don’t come back.
IMMUNOTHERAPY
This class of medications stimulates your body’s own defenses to destroy your warts.
Immunotherapy is relatively new and carried out under your doctor’s supervision.
Interferon is a chemical manufactured by human white blood cells that helps fight various infections.
Your doctor injects genetically engineered interferon directly
into a wart.
Interferon has many side effects (including high fevers, shaking chills, “flulike” symptoms) that limit its use to only five warts at a time.
Most physicians use interferon only in men who have failed less toxic treatments (podophyllin, surgery, etc.
).
The doctor injects the medication twice weekly into the base of the wart until it disappears, or for a maximum of eight weeks.
Because there are so many other less toxic treatments available, interferon should be viewed as a last resort.
Imiquimod (Aldara Cream 5%) is a physician-prescribed topical immunotherapy medication you can use in the privacy of your home.
Although we don’t know exactly how imiquimod destroys warts, it seems to stimulate people’s own natural immunity.
It works better in women than men, but in men it destroys penile warts faster than it works for perianal disease.
Men with AIDS and low T-cell counts (less than 150) should not use the medication.
Apply imiquimod to external warts only (don’t push it up into your anus) at bedtime three times a week and wash it off in the morning.
Skin reddening and irritation are common side effects that clear up if you skip an extra day between treatments.
Your warts should disappear within four months; lengthier therapy is not recommended.
SURGERY
Numerous surgical procedures to destroy venereal warts have evolved over the years, encompassing everything from the cold steel of scalpels to the high tech of lasers.
Surgeons can cut out warts or use extreme temperatures to rapidly freeze or burn them away; most often they use a combination of techniques.
Surgery works best for patients who have failed other treatments, have large bulky warts that would take too long to dissolve with topical agents, or have warts within their hard-to-treat anal canal.
Although more painful than other treatments, surgery has its advantages:
All the warts are destroyed in a single sitting
(or lying, as the case may be) and a piece is sent for biopsy to check for cancer.