Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (198 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

BOOK: Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis
10.13Mb size Format: txt, pdf, ePub
Drugs (e.g., estrogens, anabolic steroids)—most common cause (Table
5-13
)
Normal pregnancy
Alcoholic hepatitis
Infections (e.g., acute viral hepatitis, gram-negative sepsis, toxic shock syndrome, AIDS, parasitic, fungal)
Sickle cell crisis
Postoperative state following long procedure and multiple transfusions
Benign recurrent familial intrahepatic cholestasis—rare condition
Autosomal recessive condition; attacks begin after age 8, last weeks to months, complete resolution between episodes, may recur after months or years; exacerbated by estrogens
TABLE 5–13. Comparison of Various Types of Cholestatic Disease
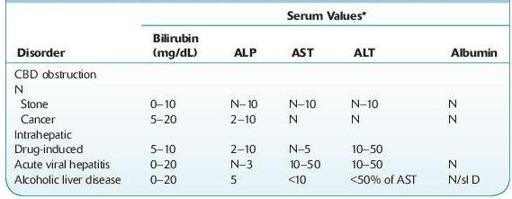
CBD, common bile duct; N, normal; sl D, slightly decreased.
*Serum value, times normal.
Laboratory Findings

Core laboratory
: Increased serum ALP, but GGT is usually normal. Serum direct bilirubin may be normal or ≤10 mg/dL. Transaminase usually <100 U.

Histology
: Liver biopsy shows centrolobular cholestasis without inflammation, bile pigment in hepatocytes and canaliculi; little or no fibrosis.
CIRRHOSIS, PRIMARY BILIARY (CHOLANGIOLITIC CIRRHOSIS, HANOT HYPERTROPHIC CIRRHOSIS, CHRONIC NONSUPPURATIVE DESTRUCTIVE CHOLANGITIS, ETC.)
Slow progressive multisystem autoimmune disease; chronic nonsuppurative inflammation and asymmetric destruction of small intrahepatic bile ducts producing chronic cholestasis, cirrhosis, and ultimately liver failure
Other books
Semper Fidelis by S.A. McAuley, T.A. Chase, Devon Rhodes, LE Franks, Sara York, Kendall McKenna, Morticia Knight
CROSSFIRE by Jenna Mills
Ms. Hannah Is Bananas! by Dan Gutman
The Brenda Diaries by Margo Candela
A Splash of Red by Antonia Fraser
París era una fiesta by Ernest Hemingway
Keep You From Harm by Debra Doxer
Runt of the Litter (Halfbreed Chronicles Book 1) by Hemlock, Isabelle
The Great Quarterback Switch by Matt Christopher
Any Place I Hang My Hat by Susan Isaacs