Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (314 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

Leukocyte alkaline phosphatase (LAP): absent or reduced.
Liver function studies: unconjugated bilirubin: increased; AST/ALT: normal; ALP: normal.
Methemalbumin: reduced.
Hemoglobin, plasma: increased (hemoglobinemia).
Urinalysis: hemoglobinuria, hemosiderinuria, and no intact RBCs in urine sediment.
Suggested Readings
Hill A, Kelly RJ, Hillmen P. Thrombosis in paroxysmal nocturnal hemoglobinuria.
Blood.
2013;121:4985–4996.
Parker CJ. Management of paroxysmal nocturnal hemoglobinuria in the era of complement inhibitory therapy.
Hematology Am Soc Hematol Educ Program.
2011;2011:21–29.
PAROXYSMAL COLD HEMOGLOBINURIA (PCH)
Definition
PCH is an acute hemolytic anemia that results from characteristic antibodies (Donath-Landsteiner) that cross-react with P blood group on RBC membrane causing osmotic lysis. This transient hemolysis occurs following exposure to a cold environment, with sudden hemoglobinuria. PCH may be associated with the convalescence phase of an acute viral illness (mumps, measles, infectious mononucleosis) or seen in patients with syphilis. PCH may also be idiopathic.
Laboratory Findings
Plasma appears scarlet and becomes maroon or brown after a few hours (free Hb is oxidized to metHb, as well as due to the formation of methemalbumin).
Peripheral blood smear (PBS): spherocytes, nucleated RBCs, anisocytosis, and poikilocytosis.
Donath-Landsteiner test: when the blood is cooled, then brought to 37°C, hemolysis develops.
Complement-directed Coombs test: may be positive but the IgG Coombs is negative.
Drug-Induced Hemolytic Anemias
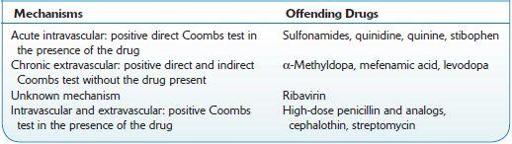
This hemolytic anemia is due to anti-RBC antibodies that develop as the result of drug effects. The drugs most commonly implicated and the mechanisms involved are described in Table
9-2
.
TABLE 9–2. Drugs Most Commonly Implicated in Hemolytic Anemias