Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (402 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

Deficiency of F XIII does not affect PT (INR), PTT, thrombin time, or fibrinogen levels.
F XIII is unaffected by vitamin K deficiency or oral anticoagulants.
Suggested Reading
Lorand L. Factor XIII and the clotting of fibrinogen: from basic research to medicine.
J Thromb Haemost.
2005;3:1337–1348.

ACQUIRED HEMORRHAGIC DISORDERS OF MULTIFACTORIAL ETIOLOGY
DISSEMINATED INTRAVASCULAR COAGULATION (DIC)
Definition
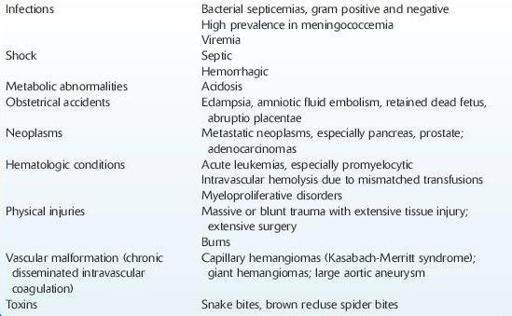
DIC is an acquired, systemic, complex syndrome, producing both hemorrhages and thrombosis. It is a secondary condition that develops as a complication to a variety of disorders (Table
9-6
).
TABLE 9–6. Common Underlying Etiologies of Disseminated Intravascular Coagulation (DIC)
DIC consists of the systemic activation of coagulation, resulting in multiple thrombi in the microcirculation, consumption of clotting proteins and platelets, in turn leading to a hemorrhagic diathesis. Intravascular fibrin deposition is the result of tissue factor–mediated thrombin generation. The fibrinolytic mechanism becomes activated in parallel, exacerbating the hemorrhagic tendency. Most cases of DIC are fulminant. In cases of chronic and low-grade DIC, blood coagulation is continuously or intermittently activated by small amounts of tissue factor, such as may be released from disseminated malignancies.
Who Should Be Suspected
In most cases of acute DIC, the condition should be suspected in an intensive care patient with end organ failure, bleeding, and thrombotic events, especially in the small vasculature and at the site of catheters. The underlying diagnosis that leads to the suspicion of acute DIC is one of the following: sepsis, trauma, cancer, obstetrical complications, and severe immunologic reactions.
Laboratory Findings
The laboratory findings of DIC are variable. They depend on the underlying etiology and stage of the syndrome. Fibrinogen, an acute-phase reactant protein, may be elevated early on but decrease progressively due to its consumption, as the condition progresses. Pathologic fibrinolysis, invariably present initially, may diminish or disappear in very severe cases when the fibrinolytic proteins are completely consumed.
Conversely, primary fibrinolysis may develop without DIC, as with direct infusion of thrombolytic agents and in a patient with prostate cancer.
Because DIC is primarily a bedside diagnosis in a severely ill patient, it should be considered when, in addition to bleeding and thrombotic events, endorgan injury is documented.
Repeated laboratory studies are more useful than a single determination. The findings described below are categorized in three groups.
1. Procoagulant activation and consumption
PT, PTT, and thrombin time may be variably prolonged but are nonspecific and hence of limited diagnostic value.