Breast Imaging: A Core Review (43 page)
Read Breast Imaging: A Core Review Online
Authors: Biren A. Shah,Sabala Mandava
Tags: #Medical, #Radiology; Radiotherapy & Nuclear Medicine, #Radiology & Nuclear Medicine

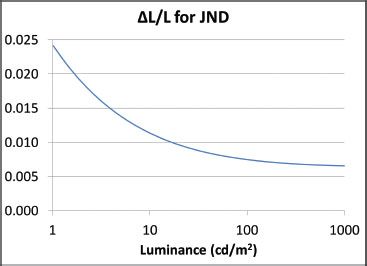
The plot of the gray-scale standard display function taken from the DICOM 14 document (
http://medical.nema.org/dicom/2004/04_14pu.pdf
) shows that for dimly luminated displays, a larger contrast is required to be perceptible than for brighter displays and so Weber law does not hold. For brighter screens (above 100 cd/m
2
), the curve flattens out to the right edge of the displayed range and beyond. (A bright mammography viewing box is 3,000 cd/m
2
) This is the situation described in the correct answer choice A.
References: Samei E. Technological and psychophysical considerations for digital mammographic displays.
Radiographics
2005;25:491–501.
8
Answer D.
Note that mean glandular dose (MGD) is the average dose throughout the breast. The dose at the beam entrance surface of the breast would be the highest. As the beam passes through the breast, it is attenuated and so the dose decreases as it passes through the breast. Thus, the average dose is lower than the dose near the beam entrance.
The problem states that the entrance exposure has increased by 60% with a 16% increase in kVp. In addition, the
penetrability
(range of x-rays in tissue) goes up with kVp (Bushong, p. 140). (This is equivalent to saying that the x-ray attenuation is less at higher kVp.) What effect does this have? It means that as the radiation passes through the tissue, it does not get reduced as much as it would at lower kVp. Thus, the mean (average) dose to the tissue is higher than it would have been had the penetrability remained constant. Thus, the dose increases by
more
than 60%.
It is important to note that according to the problem, the mAs has been held constant. Normally, if one chooses to increase the kVp, the system would automatically reduce the mAs.
Reference: Bushong SC.
Radiologic Science for Technologists
. 10th ed. St. Louis, MO: Elsevier; 2013.
9
Answer B.
CsI (indirect) is used by GE; Se (direct) is used by Hologics. BaFBr is used by FUJI (photostimulable phosphor). NaI is used in gamma cameras, not mammography.
Reference: Huda W.
Review of Radiographic Physics
. 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2010:53.
10
Answer B.
In conventional radiography (80 kV), about 2.5 to 3 cm of soft tissue attenuates half the x-ray beam; in mammography, about 1 cm of soft tissue will reduce the primary x-ray beam intensity to one half of its initial value.
Reference: Huda W.
Review of Radiographic Physics
. 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2010:54.
11
Answer C.
Currently, in digital mammography, the typical x-ray tube voltage is 30 to 32 kV, with the higher value used in thicker breasts. Twenty-five kV would be far too low, and 40 kV would be far too high.
Reference: Huda W.
Review of Radiographic Physics
. 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2010:54.
12
Answer C.
Tube currents are 100 mA for the large (0.3-mm focal spot) and only 25 mA for the small focal spot (0.1 mm); as a result, to get a given mAs in magnification mammography, the exposure time must be increased (threefold) to get the correct exposure at the image receptor.
Reference: Huda W.
Review of Radiographic Physics
. 3rd ed. Baltimore, MD: Lippincott Williams & Wilkins; 2010:54.
13
Answer C.
mAs
is an abbreviation for milliampere second, the units of measure of x-ray tube current and exposure time (Bushong, p. 593). Thus, at fixed mAs, if the exposure time goes up, the tube current must go down. At constant kVp, the dose to the breast is proportional to the mAs, which has not changed. (It has just been delivered to the breast over a longer period of time but at a lower rate.) Thus, answer choice A is incorrect. There would also be no difference in the total amount of radiation impinging on the detector and so the viewing requirements should not change. Thus, answer choice B is also incorrect. Answer choice C is the correct answer since motion blur increases with exposure time (Bushong, pp. 181, 182). A fixed mAs means that for a longer exposure time, the tube current is reduced. Thus, answer choices D and E are both wrong. If anything, since the tube current and radiation rate have both been reduced, the exposure is gentler on both the tube and the detector.
Reference: Bushong SC.
Radiologic Science for Technologists
. 10th ed. St. Louis, MO: Elsevier; 2013.
14
Answer C.
Calcium (Ca) has an atomic number of 20, whereas soft tissue has an effective atomic number of about 7.4 to 7.6. Though the attenuation coefficient drops with increasing keV for both calcifications (answer choice C) and normal breast tissue (answer choice D), the photoelectric effect for calcium is affected far more, and so the
contrast
between microcalcifications and normal breast tissue drops substantially as the photon energy increases (see Wolbarst, Fig. 33.3). Thus, the correct answer is C. Answer choice A is incorrect even though the large region of coverage for the chest radiograph might imply a decrease in resolution. Even with high resolution, we still would probably not see calcium in a chest x-ray because of the high kV. Answer choice B might be true except that the
spine
would generally not obfuscate the breasts in a chest radiograph and so this answer is easily eliminated. The range of exposure times can substantially overlap for mammograms and chest x-rays. Quite often, the exposure time will be
shorter
for a chest x-ray than for a mammogram and thus choice E is incorrect.
Reference: Wolbarst A.
Physics of Radiology
. 2nd ed. Madison, WI: Medical Physics Publishing Corp.; 2000:355–356.
15
Answer D.
Because of the air gap in magnification mammography, much of the scatter from the breast does not reach the detector. Thus, there is little scatter reduction that can be accomplished by using a grid. Yet the grid, if present, would still attenuate a significant fraction of the primary beam, requiring an increase in breast dose for the same exposure to the detector. Thus, in magnification mammography, the grid is left out since it does little good and requires more dose to the breast. (None of this is unique to mammography.) Grids
are
used in contact (nonmagnification) mammography and so answer choice A is wrong. If the grids were present, it would be moving just as it does in contact mammography and so would be just as invisible as it would be in contact mammography. Thus, answer choice B is wrong. The contrast really should not be affected by magnification and so answer choice C is wrong. Answer choice E is more or less hogwash.
Reference: Bushberg JT, Seibert JA, Leidholdt EM, et al.
The Essential Physics of Medical Imaging
. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:207–212.
16
Answer B.
Consider the geometry used for magnification mammography compared to imaging with the breast in contact with the detector. Start with the contact mammography depicted in Figure 5.1. The breast is compressed and in close contact with the detector. X-rays must penetrate through the compressed breast. As they pass through the breast, a fraction is absorbed (resulting in radiation dose to the breast.) After a sufficient amount of time, the detector receives enough radiation for an image and the automatic exposure control (AEC) turns the radiation off.

Now for the magnification mammography shown in Figure 5.2, note that the breast is still compressed (eliminating answer choice D) and the x-rays must still penetrate the same thickness of breast tissue. The same area of the detector is irradiated, and thus, the total amount of radiation received by the detector to make an image has not changed. However, the air gap in Figure 5.2 substantially reduces the amount of scatter reaching the detector while allowing all of the primary radiation to reach the detector. However, in Figure 5.1, a great deal of scatter is generated near the detector. For the geometry of Figure 5.1, this scatter would reach the detector and degrade the image and so here, a grid is used. Unfortunately, this grid also reduces the primary radiation; to make up for this, more radiation is required and thus a large focal spot is used so that this larger amount can be delivered in a comparable period of time. Thus, answer choice B is the correct answer. Answer choice A is wrong. Magnification enhances the effect of motion, not reduces it. The geometry shows that answer choice C is wrong because the density of radiation reaching the detector is what matters for making images. (If this is puzzling, think of film. The radiation density reaching the film must be the same in both cases to cause the same amount of exposure. Similar considerations apply to digital detectors.) The image of the magnified portion of the breast in Figure 5.2 will be about the same size as the image of the whole breast in Figure 5.1 and so the total radiation required by the detector should be about the same for both configurations. Finally, answer choice E is wrong because the overall image quality needs to be the same for both situations. (Thought question? What are the implications for radiation dose to the breast for both 1 and 2? What are the implications for total amount of radiation absorbed by the breast for both 1 and 2?)
Reference: Bushberg JT, Seibert JA, Leidholdt EM, et al.
The Essential Physics of Medical Imaging
. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:207–212.
17
Answer A.
First consider answer choices C, D, and E. Answer choice C is wrong because tissue contrast decreases with increased kV (Wolbarst, Fig. 33.3, p. 356). In considering answer choice D, the spatial resolution can actually improve some at moderate and higher kV because at low kV, a phenomenon called “blooming” can become significant (Wolbarst, p. 290). This occurs because at lower kV, the electrons traveling from the cathode to anode have a little more time to repel each other and spread apart more, slightly increasing the effective size of the focal spot. Increasing the kV beyond 26 or so does not improve things much and so this is generally not an important effect (and has nothing to do with breast thickness). Scatter itself generally increases with kV, not decreases (Wolbarst, p. 314) and so choice E is wrong.
This leaves answer choices A and B. The correct answer is A. Higher penetration allows for a shorter exposure time. (If possible, the exposure time should be kept below 2 seconds. Discuss this with mammography radiologists for more insight.) Though answer choice B is also true the most important reason is to keep the exposure time down to reduce motion artifacts.
Reference: Wolbarst A.
Physics of Radiology
. 2nd ed. Madison, WI: Medical Physics Publishing Corp.; 2000.
18
Answer C.
Xeroradiography is no longer available but had breast doses greater than film-screen. Both CR and digital mammogram are about 30% less than that for film-screen with direct digital almost one-half of film-screen.
Other books
King's Mountain by Sharyn McCrumb
Finding Hope by Broas, K
Dunk Under Pressure by Rich Wallace
Dire Sparks (Song of the Aura, Book Five) by Downs, Gregory J.
The Force Unleashed by Sean Williams
The Mystic Marriage by Jones, Heather Rose
Mine to Keep by Cynthia Eden
The Redhunter by William F. Buckley
American Buffalo by Steven Rinella