Fundamentals of Midwifery: A Textbook for Students (103 page)
Read Fundamentals of Midwifery: A Textbook for Students Online
Authors: Louise Lewis

BOOK: Fundamentals of Midwifery: A Textbook for Students
5.14Mb size Format: txt, pdf, ePub
241
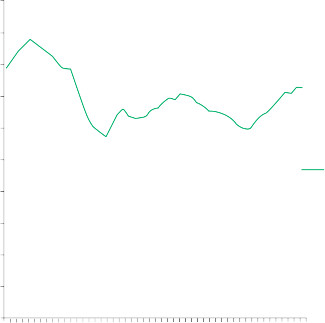
1,000,000
900,000
800,000
700,000
600,000

242
500,000
400,000
300,000
200,000
100,000
1960
1963
1966
1969
1972
1975
1978
1981
1984
1987
1990
1993
1996
1999
2002
2005
2008
2011
0
Number of live births
Figure 11.4
Graph showing number of live births in the England and Wales over a 50-year period (between 1961 and 2011) (ONS, 2012c).
Table 11.1
Maternal and infant deaths
Measure
Definition
Stillbirth
Since 1992: a child born from the 24th completed week of gestation, who never showed any signs of life.
Stillbirth rate
Number of stillbirths per 1000 total births (live births plus stillbirths).
Early neonatal deaths
Deaths under seven days.
Perinatal deaths
Stillbirths and early neonatal deaths.
Maternal mortality
The death of a woman within 42 days of the end of pregnancy from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes.
Maternal mortality rate
Number of maternal deaths of mothers, from direct and indirect causes, within the first 42 days after the end of pregnancy per 100,000 maternities (pregnancies).
Maternal mortality ratio
Number of maternal deaths of mothers, from direct and indirect causes, within the first 42 days after the end of per 100,000 live births.
Neonatal deaths
Deaths under 28 days.
Post-neonatal deaths
Deaths between 28 days and 1 year.
Infant deaths
Deaths under 1 year.
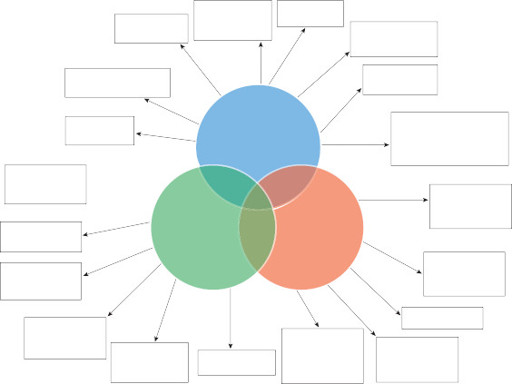
Domains of public health
The UK Faculty of Public Health (2010) has identified three interrelated domains of public health
(see Figure 11.5) (Griffiths et al. 2005). These are:
health improvement
health protection
health services (quality improvement).
Health improvement
concerns socioeconomic aspects, health promotion, and determinants of health (Thorpe et al. 2008). This encompasses reducing health inequalities in partnership with multiple sectors (Griffiths et al. 2005).
Health protection
includes the control of infectious and communicable diseases and environmental hazards; strategies include immunisation pro- grammes (Thain and Hickman 2004).
Health service (quality improvement)
relates to the role of healthcare systems, service planning and quality, clinical effectiveness, clinical governance and health economics. These include prioritisation and equity of services, clinical audit, evaluation and research (Thorpe et al. 2008; UK’s Faculty of Public Health 2010).
 243
243
 HealthEducationHousingFamily/communityinequalities
HealthEducationHousingFamily/communityinequalities
Health
promotion EmploymentLifestyles
Health improvement
Surveillance and monitoring of disease and risk factorsClinical effectivenessEfficiencyService planning
Improving (health) services
Health protection
Infectious diseasesChemicals and poisonsAudit and evaluationsClinical governanceEquityEnvironmental health hazardsRadiationEmergency response
Figure 11.5
Diagram illustrating the three domains of public health and the scope of public health practice.244
Health improvement: the midwife and health promotion
Health promotion is defined as activities designed to maintain optimum health and quality oflife for groups of people; these involve engaging the community in their personal health whether individually or collectively (Martin 2010). Childbirth, as a normal life event, fits within a health promotion framework (Beldon and Crozier 2005). Health education uses persuasive methods to inform groups or individuals about adopting healthier lifestyles and rejecting unhealthy habits; the educator determines what changes will be beneficial for the population (Martin 2010). Piper (2005) proposes four categories of health promotion strategies used by midwives; these are the
behaviour change agent
, the
collective empowerment facilitator
,
strategic practitioner
and
collective empowerment
facilitator (see Figure 11.6).
 The
The
behaviour change agent
, or
health persuasion
approach uses health education where an expert clinician (e.g. midwife) identifies areas within the medical model of health requiring change in the recipients of care (Piper 2005). Disease prevention is emphasised, using orthodox medical approaches (Furber 2000; Whitehead 2003). Pregnancy is seen as the pre-eminent ‘
teachable moment
’ (Herzig et al. 2006, p. 230): women are highly motivated and responsive, within a context of relatively intensive and continuous care from health professionals. Preventa- tive measures may be
primary, secondary
or
tertiary
, these relate respectively to avoidance of disease (or wider public health problems), control of an identified condition, or preventing worsening of an identified issue.An
empowerment facilitator
uses non-coercive, democratic, women-centred methods to achieve health promotion through constructive partnership with women (e.g. in the use of the
Objective knowledge emphasis
Midwife as expert and midwife focussed intervention
The midwife as behaviour change agent
The midwife as strategic practitioner
Individual woman focus
Women (population) focus
The midwife as empowerment facilitator
The midwife as collective empowerment facilitator
Subjective knowledge emphasis
Women as experts and women focused intervention
Figure 11.6
Diagram displaying the difference between models of health promotion (Piper 2005).expert patient, patient advice, liaison services and engagement of service users (Piper 2005). A
strategic practitioner
uses the legislative action to evaluate wider socio-political issues which affect the health of individuals, but are beyond their direct control. These include, health in- equalities and unequal distribution of wealth and capital (Furber 2000; Piper 2005). This is a top-down approach to health promotion. The
collective empowerment facilitator
employs the ‘community development method’ of health promotion (Furber 2000; Piper 2005), focusing on societal factors as the main determinant of health. However, these operate a bottom-up approach, responding to the collectively expressed, subjective health needs of women and their families. Examples include the facilitation of peer support schemes for mothers, such as breast- feeding drop-in peer support groups (Piper 2005).
Health surveillance
Health surveillance aims to, ‘
provide the right information, at the right time, in the right place to
inform decision-making and action-taking
’ (DH 2013a, p. 5). Screening is part of health surveil- lance which is part of routine antenatal midwifery care. Screening is where apparently healthy members of a population are assessed for their susceptibility to diseases and conditions (Tiran 2008; Martin 2010). Antenatal screening may include determining a mother’s carrier status for recessive genetic disorders, which the baby could inherit or the mother’s susceptibility to certain infectious diseases. UK childbearing women are offered a programme of routine antenatal screening and diagnostic testing in pregnancy for certain infectious diseases in the mother, which may be at a pre-clinical stage, but still infectious (Tiran 2008; Porth 2009; Martin 2010). Additional screening and diagnostic testing are made available when there is a clear history of exposure or susceptibility. This programme aims to improve health outcomes in the population of childbearing women and their babies (see Chapter 6: ‘Antenatal midwifery care’, where ante- natal screening is discussed in greater depth).
Improving health services through clinical audit: confidential enquiries into maternal and child health
A major way in which clinical audit has been used to inform maternal public health is the Con-fidential Enquiries into maternal deaths instituted in the UK in 1952 and subsequently infant mortality (Weindling 2003; Kee 2005). These gather statistical data on maternal and infant mor- tality over a three year period (e.g. Centre for Maternal and Child Enquiries (CMACE) 2011). These enquiries revealed key areas of risk, compelling midwives to act to reduce maternal mortality in relation to key issues including:
Health improvement
concerns socioeconomic aspects, health promotion, and determinants of health (Thorpe et al. 2008). This encompasses reducing health inequalities in partnership with multiple sectors (Griffiths et al. 2005).
Health protection
includes the control of infectious and communicable diseases and environmental hazards; strategies include immunisation pro- grammes (Thain and Hickman 2004).
Health service (quality improvement)
relates to the role of healthcare systems, service planning and quality, clinical effectiveness, clinical governance and health economics. These include prioritisation and equity of services, clinical audit, evaluation and research (Thorpe et al. 2008; UK’s Faculty of Public Health 2010).
 243
243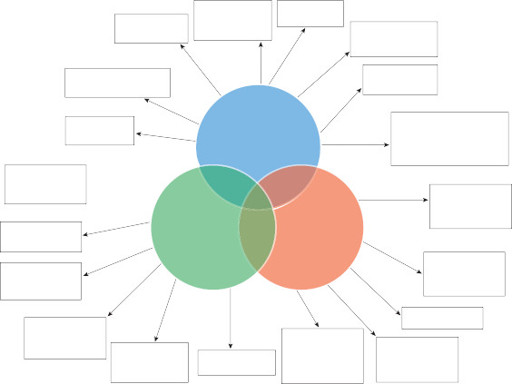 HealthEducationHousingFamily/communityinequalities
HealthEducationHousingFamily/communityinequalitiesHealth
promotion EmploymentLifestyles
Health improvement
Surveillance and monitoring of disease and risk factorsClinical effectivenessEfficiencyService planning
Improving (health) services
Health protection
Infectious diseasesChemicals and poisonsAudit and evaluationsClinical governanceEquityEnvironmental health hazardsRadiationEmergency response
Figure 11.5
Diagram illustrating the three domains of public health and the scope of public health practice.244
Health improvement: the midwife and health promotion
Health promotion is defined as activities designed to maintain optimum health and quality oflife for groups of people; these involve engaging the community in their personal health whether individually or collectively (Martin 2010). Childbirth, as a normal life event, fits within a health promotion framework (Beldon and Crozier 2005). Health education uses persuasive methods to inform groups or individuals about adopting healthier lifestyles and rejecting unhealthy habits; the educator determines what changes will be beneficial for the population (Martin 2010). Piper (2005) proposes four categories of health promotion strategies used by midwives; these are the
behaviour change agent
, the
collective empowerment facilitator
,
strategic practitioner
and
collective empowerment
facilitator (see Figure 11.6).
 The
Thebehaviour change agent
, or
health persuasion
approach uses health education where an expert clinician (e.g. midwife) identifies areas within the medical model of health requiring change in the recipients of care (Piper 2005). Disease prevention is emphasised, using orthodox medical approaches (Furber 2000; Whitehead 2003). Pregnancy is seen as the pre-eminent ‘
teachable moment
’ (Herzig et al. 2006, p. 230): women are highly motivated and responsive, within a context of relatively intensive and continuous care from health professionals. Preventa- tive measures may be
primary, secondary
or
tertiary
, these relate respectively to avoidance of disease (or wider public health problems), control of an identified condition, or preventing worsening of an identified issue.An
empowerment facilitator
uses non-coercive, democratic, women-centred methods to achieve health promotion through constructive partnership with women (e.g. in the use of the
Objective knowledge emphasis
Midwife as expert and midwife focussed intervention
The midwife as behaviour change agent
The midwife as strategic practitioner
Individual woman focus
Women (population) focus
The midwife as empowerment facilitator
The midwife as collective empowerment facilitator
Subjective knowledge emphasis
Women as experts and women focused intervention
Figure 11.6
Diagram displaying the difference between models of health promotion (Piper 2005).expert patient, patient advice, liaison services and engagement of service users (Piper 2005). A
strategic practitioner
uses the legislative action to evaluate wider socio-political issues which affect the health of individuals, but are beyond their direct control. These include, health in- equalities and unequal distribution of wealth and capital (Furber 2000; Piper 2005). This is a top-down approach to health promotion. The
collective empowerment facilitator
employs the ‘community development method’ of health promotion (Furber 2000; Piper 2005), focusing on societal factors as the main determinant of health. However, these operate a bottom-up approach, responding to the collectively expressed, subjective health needs of women and their families. Examples include the facilitation of peer support schemes for mothers, such as breast- feeding drop-in peer support groups (Piper 2005).
Health surveillance
Health surveillance aims to, ‘
provide the right information, at the right time, in the right place to
inform decision-making and action-taking
’ (DH 2013a, p. 5). Screening is part of health surveil- lance which is part of routine antenatal midwifery care. Screening is where apparently healthy members of a population are assessed for their susceptibility to diseases and conditions (Tiran 2008; Martin 2010). Antenatal screening may include determining a mother’s carrier status for recessive genetic disorders, which the baby could inherit or the mother’s susceptibility to certain infectious diseases. UK childbearing women are offered a programme of routine antenatal screening and diagnostic testing in pregnancy for certain infectious diseases in the mother, which may be at a pre-clinical stage, but still infectious (Tiran 2008; Porth 2009; Martin 2010). Additional screening and diagnostic testing are made available when there is a clear history of exposure or susceptibility. This programme aims to improve health outcomes in the population of childbearing women and their babies (see Chapter 6: ‘Antenatal midwifery care’, where ante- natal screening is discussed in greater depth).
Improving health services through clinical audit: confidential enquiries into maternal and child health
A major way in which clinical audit has been used to inform maternal public health is the Con-fidential Enquiries into maternal deaths instituted in the UK in 1952 and subsequently infant mortality (Weindling 2003; Kee 2005). These gather statistical data on maternal and infant mor- tality over a three year period (e.g. Centre for Maternal and Child Enquiries (CMACE) 2011). These enquiries revealed key areas of risk, compelling midwives to act to reduce maternal mortality in relation to key issues including:
Other books
Operation Napoleon by Arnaldur Indriðason
Towards a Dark Horizon by Maureen Reynolds
Shifters by Lee, Edward
A Potion to Die For: A Magic Potion Mystery by Blake, Heather
The Marriage Bed (The Medieval Knights Series) by Dain, Claudia
Hybrid: Savannah by Ruth D. Kerce
All in the Family by Taft Sowder
Wired for Culture: Origins of the Human Social Mind by Mark Pagel
The Pearl Savage by Tamara Rose Blodgett
Snapshot by Angie Stanton