Fundamentals of Midwifery: A Textbook for Students (104 page)
Read Fundamentals of Midwifery: A Textbook for Students Online
Authors: Louise Lewis

BOOK: Fundamentals of Midwifery: A Textbook for Students
12.18Mb size Format: txt, pdf, ePub
sepsis (see Chapter 8)
serious illness (see Chapter 16)
smoking
mental health (see Chapters 4 and 13)
obesity
age (younger and older mothers) (see Chapter 5)
ethnicity
asylum status
literacy
 245
245
Table 11.2
Social class definitions used in the Black Report (1980)
 Class definition
Class definition
Descriptions
Percentage of the population in 1980
I. (Professional)Professional (e.g. accountant, doctor, lawyer)5%Ii. (Intermediate)Intermediate (e.g. manager, schoolteacher, nurse)18%Iiin. (Skilled, Non-Manual)Skilled non-manual (e.g. clerical worker, secretary, shop assistant)12%Iilm. (Skilled, Manual)Skilled manual (e.g. bus driver, butcher, coal face worker, carpenter)38%IV. (Partly Skilled)Partly skilled (e.g. agricultural worker, bus conductor, postman)18%V. (Unskilled)Unskilled (e.g. labourer, cleaner, dock worker)9%246
 245
245Table 11.2
Social class definitions used in the Black Report (1980)
 Class definition
Class definitionDescriptions
Percentage of the population in 1980
I. (Professional)Professional (e.g. accountant, doctor, lawyer)5%Ii. (Intermediate)Intermediate (e.g. manager, schoolteacher, nurse)18%Iiin. (Skilled, Non-Manual)Skilled non-manual (e.g. clerical worker, secretary, shop assistant)12%Iilm. (Skilled, Manual)Skilled manual (e.g. bus driver, butcher, coal face worker, carpenter)38%IV. (Partly Skilled)Partly skilled (e.g. agricultural worker, bus conductor, postman)18%V. (Unskilled)Unskilled (e.g. labourer, cleaner, dock worker)9%246
substance misuse
domestic abuse. (Jewell 2005; Lewis 2007; Centre for Maternal and Child Enquiries (CMACE)2011)
Health inequalities
DH (2007, p. 16) stated:
. . . Health inequalities stem from inequalities in people’s early life experience, their education and occupational status, exposure to lifestyle and the environmental risks and diseases to which their life courses predispose them. People in disadvantaged groups and areas tend to experience the poorest health . . .
The Black Report (1980) identified the persistence of inequalities in health between people of different social classes in the UK, despite major health service reforms and advancements. These included higher mortality rates, lower life expectancy, and lower birth weight of infants, for people in social classes IV and V (Table 11.2). Some of this could be attributed to different habits and lifestyle choices of people in different social classes. Cancer Research UK (2011) reported the persistently higher prevalence of smoking among manual workers, compared with non-manual workers (see Figure 11.7). The European Foundation for the Improvement of Living and Working Conditions (2003) reported links between poverty and ill health (see Figure 11.8) and showed that lower income areas had demonstrably poorer health outcomes. Complex relationships exist between wealth, employment and ill-health which contribute to the polarisa- tion of health outcomes in different social classes (see Figure 11.9). Similarly, Osmond et al. (1989) showed that place of birth predicted likelihood of future ill-health, independent of current place of residence. This featured in the seminal work ‘Fetal and Infant Origins of Adult Disease’ (Barker 1989) showing correlations between events in early life, and the development of chronic ill health in later life (e.g. type-2 diabetes mellitus and coronary heart disease, result- ing in lower life expectancy). Maternal health status and infant nutrition were implicated in shaping outcomes for offspring (Barker 1997; Barker 2001; Morley 2006). Social class is also cor- related with relative breastfeeding initiation and continuation rates (see Chapter 10: ‘Infant feeding’, where socio-economic influences on infant feeding choices are discussed in greater depth).
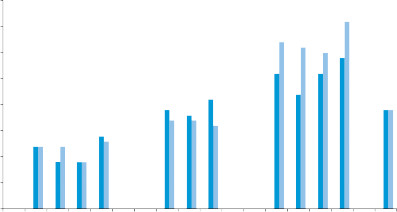 403530
403530
Percentage
252015
 Women 2011%
Women 2011%
 10 Women 2012%5RoutineTotal0
10 Women 2012%5RoutineTotal0
 Managerial & professionalHigher professionalLower managerial & professionalIntermediateIntermediateSmall employers & own accountRoutine & manualLower supervisory & technicalSemi-routine247Large employers & high managerial
Managerial & professionalHigher professionalLower managerial & professionalIntermediateIntermediateSmall employers & own accountRoutine & manualLower supervisory & technicalSemi-routine247Large employers & high managerial
Occupation
Figure 11.7
The relationship between occupation and prevalence of smoking, in women 2011 and 2012 (ONS, 2013).

 lll health
lll health
 Poverty
Poverty
Figure 11.8
Diagram illustrating the relationship between poverty and ill health.The Acheson Report (1998) made recommendations for supporting healthy maternal and child nutrition and reducing risks to children through unhealthy maternal lifestyles, such as smoking in pregnancy and maternal obesity, geared towards positively influencing the long term health of children and adults. These recommendations were reflected in the NHS Plan (Department of Health (DH) (2000), identifying midwives as an integral part of its public health strategy. A strong public health focus, involving midwives within maternal and child health services, was preserved throughout the New Labour administration. The National Service Frameworks (NSF) for Children, Young People and Maternity Services (DH 2004) placed a strong emphasis on health promotion, from pre-conceptual stages, pregnancy, childhood, through to adulthood. Strategies included high quality care throughout pregnancy and the initiation of ‘
Sure Start
’ programmes in order to deliver public health targets. Community midwives’ reloca- tion to Children’s Centres enhanced their visibility and accessibility to local communities, with the intention of reducing health inequalities (DH 2004).
Determinants of health
Health inequalities are related to wider societal factors defined by Dahlgren and Whitehead(1992) as ‘Determinants of Health’. A person’s individual characteristics, such as genetic make
 Employment (conditions & environment)lll health
Employment (conditions & environment)lll health
 248PovertyUnemployment
248PovertyUnemployment
Figure 11.9
Diagram illustrating the possible relationships between poverty, ill-health and employment.up, sex and age are central. These are then influenced by multiple factors, including lifestyle choices and living and working conditions. When discussing each of the issues below it is important to remember that many of these do not occur in isolation from one another, in any childbearing woman. For example, socioeconomic status and ethnicity is related to both smoking and obesity. Some of these are interrelated complex social needs in one woman, such as: domestic abuse, young motherhood, substance misuse and mental illnesses. Women who do not speak English have been identified as having complex social needs; they and their chil- dren have poor perinatal health outcomes (CMACE 2010; NICE 2010a). It should also become apparent that there is much overlap between the different domains of public health.
Guidance for public health
The National Institute for Clinical Excellence (NICE) was established in 1999, as a special healthauthority ensuring better consistency in availability and quality of NHS treatments and care. Following a merger with the Health Development Agency in 2005, NICE became the National Institute for
Health
and Clinical Excellence incorporating public health guidance, for preventing ill health and promoting healthier lifestyles. Numerous NICE guidelines focus on the care of childbearing women and babies (Table 11.3). In April (2013) NICE became the National Institute for Health and Care Excellence. Public Health England was established in 2013 to ‘
Health inequalities
DH (2007, p. 16) stated:
. . . Health inequalities stem from inequalities in people’s early life experience, their education and occupational status, exposure to lifestyle and the environmental risks and diseases to which their life courses predispose them. People in disadvantaged groups and areas tend to experience the poorest health . . .
The Black Report (1980) identified the persistence of inequalities in health between people of different social classes in the UK, despite major health service reforms and advancements. These included higher mortality rates, lower life expectancy, and lower birth weight of infants, for people in social classes IV and V (Table 11.2). Some of this could be attributed to different habits and lifestyle choices of people in different social classes. Cancer Research UK (2011) reported the persistently higher prevalence of smoking among manual workers, compared with non-manual workers (see Figure 11.7). The European Foundation for the Improvement of Living and Working Conditions (2003) reported links between poverty and ill health (see Figure 11.8) and showed that lower income areas had demonstrably poorer health outcomes. Complex relationships exist between wealth, employment and ill-health which contribute to the polarisa- tion of health outcomes in different social classes (see Figure 11.9). Similarly, Osmond et al. (1989) showed that place of birth predicted likelihood of future ill-health, independent of current place of residence. This featured in the seminal work ‘Fetal and Infant Origins of Adult Disease’ (Barker 1989) showing correlations between events in early life, and the development of chronic ill health in later life (e.g. type-2 diabetes mellitus and coronary heart disease, result- ing in lower life expectancy). Maternal health status and infant nutrition were implicated in shaping outcomes for offspring (Barker 1997; Barker 2001; Morley 2006). Social class is also cor- related with relative breastfeeding initiation and continuation rates (see Chapter 10: ‘Infant feeding’, where socio-economic influences on infant feeding choices are discussed in greater depth).
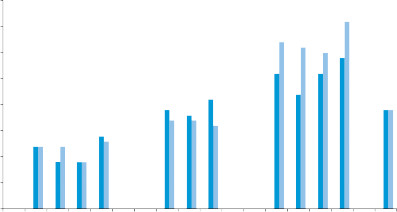 403530
403530Percentage
252015
 Women 2011%
Women 2011% 10 Women 2012%5RoutineTotal0
10 Women 2012%5RoutineTotal0 Managerial & professionalHigher professionalLower managerial & professionalIntermediateIntermediateSmall employers & own accountRoutine & manualLower supervisory & technicalSemi-routine247Large employers & high managerial
Managerial & professionalHigher professionalLower managerial & professionalIntermediateIntermediateSmall employers & own accountRoutine & manualLower supervisory & technicalSemi-routine247Large employers & high managerialOccupation
Figure 11.7
The relationship between occupation and prevalence of smoking, in women 2011 and 2012 (ONS, 2013).

 lll health
lll health Poverty
PovertyFigure 11.8
Diagram illustrating the relationship between poverty and ill health.The Acheson Report (1998) made recommendations for supporting healthy maternal and child nutrition and reducing risks to children through unhealthy maternal lifestyles, such as smoking in pregnancy and maternal obesity, geared towards positively influencing the long term health of children and adults. These recommendations were reflected in the NHS Plan (Department of Health (DH) (2000), identifying midwives as an integral part of its public health strategy. A strong public health focus, involving midwives within maternal and child health services, was preserved throughout the New Labour administration. The National Service Frameworks (NSF) for Children, Young People and Maternity Services (DH 2004) placed a strong emphasis on health promotion, from pre-conceptual stages, pregnancy, childhood, through to adulthood. Strategies included high quality care throughout pregnancy and the initiation of ‘
Sure Start
’ programmes in order to deliver public health targets. Community midwives’ reloca- tion to Children’s Centres enhanced their visibility and accessibility to local communities, with the intention of reducing health inequalities (DH 2004).
Determinants of health
Health inequalities are related to wider societal factors defined by Dahlgren and Whitehead(1992) as ‘Determinants of Health’. A person’s individual characteristics, such as genetic make
 Employment (conditions & environment)lll health
Employment (conditions & environment)lll health 248PovertyUnemployment
248PovertyUnemploymentFigure 11.9
Diagram illustrating the possible relationships between poverty, ill-health and employment.up, sex and age are central. These are then influenced by multiple factors, including lifestyle choices and living and working conditions. When discussing each of the issues below it is important to remember that many of these do not occur in isolation from one another, in any childbearing woman. For example, socioeconomic status and ethnicity is related to both smoking and obesity. Some of these are interrelated complex social needs in one woman, such as: domestic abuse, young motherhood, substance misuse and mental illnesses. Women who do not speak English have been identified as having complex social needs; they and their chil- dren have poor perinatal health outcomes (CMACE 2010; NICE 2010a). It should also become apparent that there is much overlap between the different domains of public health.
Guidance for public health
The National Institute for Clinical Excellence (NICE) was established in 1999, as a special healthauthority ensuring better consistency in availability and quality of NHS treatments and care. Following a merger with the Health Development Agency in 2005, NICE became the National Institute for
Health
and Clinical Excellence incorporating public health guidance, for preventing ill health and promoting healthier lifestyles. Numerous NICE guidelines focus on the care of childbearing women and babies (Table 11.3). In April (2013) NICE became the National Institute for Health and Care Excellence. Public Health England was established in 2013 to ‘
Other books
Red Hot Obsessions by Blair Babylon
Stolen by Rebecca Muddiman
Angst (Book 4) by Robert P. Hansen
Team Lucas (The Saints Team #1) by Ally Adams
Civil War Stories by Ambrose Bierce
The First Wife by Erica Spindler
Kent Conwell - Tony Boudreaux 08 - Death in the French Quarter by Kent Conwell
Midnight Sun by Jo Nesbo
Further Adventures by Jon Stephen Fink
The Eyes of the Dead by Yeates, G.R.