i bc27f85be50b71b1 (98 page)
Read i bc27f85be50b71b1 Online
Authors: Unknown

Headache, seizure,
Headache, vomiting, altered
findings
cranial nerve palsy
brain stem reflexes
Source: D:1(:I from JV Hickey. Thc Clinical Practice of Neurological and Neurosurgical
NurSIng (41h cd). Philadelphia: Lippincott, 1997.
outlined in Table 4-2 1 . Appendix Table llI-A.5 describes the different
types of ICP monitoring systems.
Cerebral perfusion pressure (CPP), or cerebral blood pressure, is
mean arterial pressure minus ICP. It indicares oxygen delivery to the
brain. Normal CPP is 70-100 mm Hg. CPPs at or less than 60 mm
Hg for a prolonged length of time correlate with ischemia and anoxic
brain injury.46
Following are terms related to ICP:
Brain herniatioll. The displacement of brain parenchyma through an
anaromic opening; named according ro the location of the displaced Structure (e.g., lranslelltorial herniation is the herniation of the cerebral hemispheres, diencephalon, or midbrain beneath the
tentorium cerebelli)
Mass effect. The combination of midline shift, third ventricle compression, and hydrocephalus8

324 ACUTE CARE HANDBOOK FOR PHYSICAL THERAPISTS
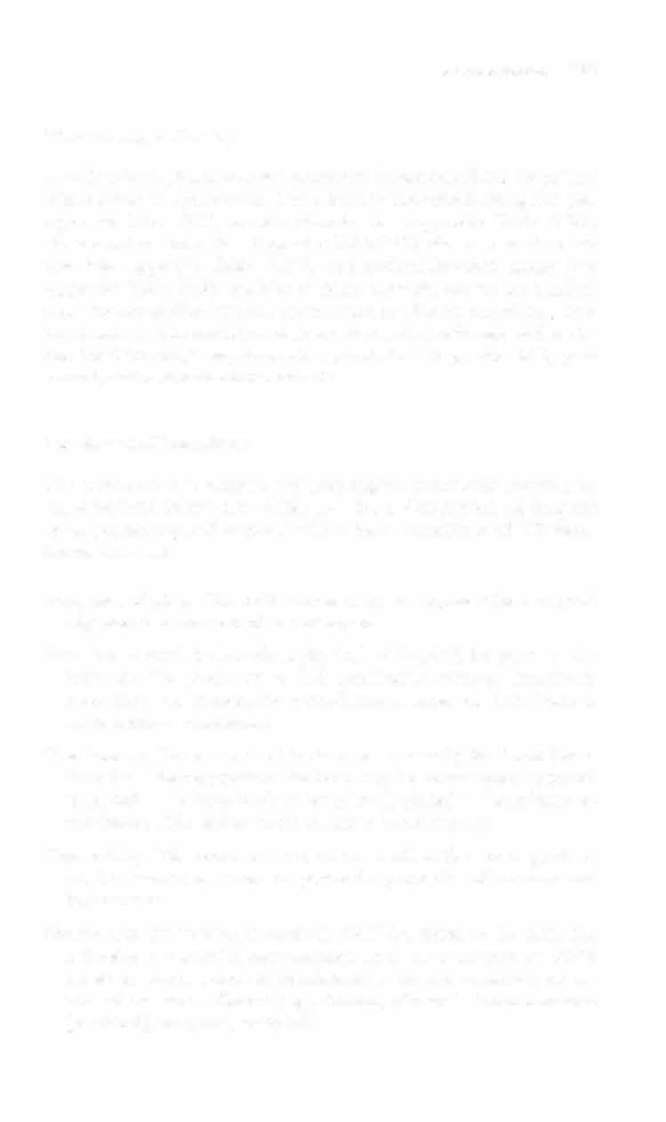
Table 4-2 1 . Treatment Options to Decrease Intracranial Pressure (1CP)
Variable
Treatment
Blood pressure
Inotropic drugs to maintain mean arterial pressure
>90 mm Hg to aid in cerebral perfusion, or antihypertensives
Osmorherapy
Osmotic diuretic to minimize cerebral edema
Mechanical
Normocapnia· to maximize cerebral oxygen delivery
ventilation
by limiting cerebral ischemia from the vasoconstrictive effects of decreased Paco2
Cerebrospinal
Ventriculostomy to remove cerebrospinal fluid
fluid drainage
Seda tion/paral ysis
Barbiturates to decrease cerebral blood flow or ocher
medication to decrease the stress of noxious activities
Positioning
Head of the bed at 30-45 degrees to increase cerebral
venous drainage
Promote neutral cervical spine and head position
Environment
Dim lights, decreased noise, frequent rest periods to
decrease external stimulation
Seizure control
Prophylactic anticonvulsant medication
Temperature
Normothermia or induced hypothermia to 32-35°C
control
(e.g., cooling blanket or decreased room temperature)
to decrease cerebral metabolism
· Routine aggressive hyperventilation is no longer used for the control of elevated ICP.
Hyperventilarion can contribute to secondary brain injury because of a rebound
increase in cerebral blood flow and volume in response to a decreased cerebrospinal
fluid pH.
Source: Data from F Wong. Prevemion of secondary brain injury. Crit Care Nurs
2000;20, 18-27.
Midlille shift. The lateral displacement of the falx cerebri secondary
to a space-occupying lesion
Space-occupying lesion. A mass lesion, such as a rumor or hematoma,
that displaces brain parenchyma and may result in the elevation of
ICP and shifting of the brain
Another primary goal of the team is to prevent further neurologic
impairment. The main components of management of the patient with
neurologic dysfunction in the acute care setting include pharmacologic
therapy, surgical procedures, and physical therapy intervention.
NERVOUS SYSTEM
325
Phamtacologic Therapy
A multitude of pharmacologic agents can be prescribed for the patient
with neurologic dysfunction. These include anticonvulsant agents (see
Appendix Table IV.5), osmotic diuretics (see Appendix Table lV.26),
adrenocorricosteroids (see Appendix Table lV. I ), skeletal muscle relaxants (see Appendix Table lV.28), and anti parkinsonian agents (see Appendix Table IV.9). Additional pharmacologic agents for medical
needs include antibiotics (e.g., for infection or after neurosurgery), antihypertensives, thrombolytics, anticoagulants, chemotherapy and radiation for CNS neoplasm, stress ulcer prophylaxis (e.g., after SCI), pain control, and neuromuscular blockade.
Neurosurgical Procedures
The most common surgical and nonsurgical neurologic procedures
arc described below (see Table 3-8 for a description of surgical
spine procedures and Appendix I II-A for a description of ICP monitoring devices).
Allellryslll clippillg. The obliteration of an aneutysm with a surgical
clip placed at the stem of the aneurysm.
Bllrr hole. A small hole made in the skull with a drill for access to the
brain for the placement of ICP monitoring systems, hematoma
evacuation, or stereotactic procedures; a series of burr holes is
made before a craniotomy.
Cralliectomy. The removal of incised bone, usually for brain (bone
Aapl tissue decompression; the bone may be permanently removed
or placed in the bone bank Or temporarily placed in the subcutaneous tissue of the abdomen (to maintain blood supply).
Crallioplasty. The reconstruction of the skull with a bone graft or
acrylic material to restore the protective properties of the scalp and
for cosmesis.
Cralliotomy. An incision through the skull for access to the brain for
extensive intracranial neurosurgery, such as aneurysm or AVM
repair or tumor removal; craniotomy is named according to the
area of the bone affecred (e.g., frontal, bifrontal, frontotemporal
[pterional], temporal, occipital).


326 ACUTE CARE HANDBOOK FOR PHYSICAl THERAPISTS
Embolization. The use of arrerial catheterization (entrance usually at
the femoral artery) to place a material, such as a detachable coil,
balloon, or sponge, to clot off an AVM or aneurysm.
Evacuation. The removal of an epidural, subdural, or intraparenchymal hematoma via burr hole or cranioromy.
Shunt placement. The insertion of a shunt system that connects the
ventricular system with the right atrium (VA shunt) or peritoneal
caviry (VP shunt) to allow the drainage of CSF when ICP rises.
Stereotaxis. The use of a stereotactic frame (a frame that temporarily
attaches ro the patient's head) in conjunction with head CT results
to specifically localize a pretargeted site, as in tumor biopsy; a burr
hole is then made for access to the brain.
Clinical Tip
• The physical therapist should be aware of the location
of a craniectomy, because the patient should nOt have
direct pressure applied to thar area. Look for signs posted
at the patient's bedside that communicate positioning
restrictions.
•
Pay close attention to head of bed positioning restricrions for the patient who has recently had neurosurgery.