Pediatric Primary Care (69 page)

vi. Fever.
vii. Nuchal rigidity and other signs of meningeus may be present if upper lobes are involved.
viii. Drowsiness, restlessness.
ix. Respiratory distress and hypoxemia are variable or mild without widespread disease or pleural effusion.
3.
M. pneumoniae.
a. Fever.
b. Diminished breath sounds; coarse, harsh breath sounds.
c. May have macular rash, erythematous macular rash, urticaria.
d. Cervical lymphadenopathy.
e. Conjunctivitis, otitis media.
f. Arthropathy.
E. Diagnostic tests.
1. Viral pneumonia.
a. Definitive diagnosis: viral isolation/viral antigens in respiratory tract infection.
b. CXR: typically shows bilateral, diffuse infiltrates.
c. WBC: normal or leukocytosis (not usually 20,000) with lymphocytosis.
2. Bacterial pneumonia.
a. No “gold standard” definitive test.
b. Blood cultures are positive for the causative agent only about 10% of the time.
c. WBC: leukocytosis (15,000-40,000) with granulocytosis.
d. CXR.
•
S. pneumoniae:
lobar consolidation; typically single focus but may be multiple foci; “spherical” infiltrate or round pneumonia; right lobes are preferentially affected.
•
S. aureus:
bronchopneumonia (multiple, central segmental infiltrates become confluent and diffuse); these infiltrates lead to necrosis, cavitation, pneumatoceles, and abscess formation.
3.
M. pneumoniae.
a. Clinical manifestation and physical exam are essential to diagnosis.
• Insidious onset, nontoxic.
• Child older than 5 years of age.
• Low-grade fever.
b.
M. pneumoniae
detected by polymerase chain reaction (PCR) technology.
c. Cold agglutinins (during acute phase) with titer 1:64 or greater are predictive of
M. pneumoniae.
d. WBC: normal.
F. Differential diagnosis.
| A spirations, 934.8 | Foreign body aspiration, 934.8 |
| Asthma, 493.9 | Mycoplasma pneumoniae, 483 |
| Bronchiolitis, 466.49 | Pneumonia, viral, 480.9 |
| Coryza, 460 | Tracheoesophageal fi stula, 530.84 |
| Cystic fibrosis, 277 | Upper respiratory infection, 465.9 |
| Fever, 780.6 |
1. Viral pneumonia: URI symptoms and coryza with low-grade fever; bacterial pneumonia: abrupt onset with high fever;
M. pneumoniae:
insidious onset and nontoxic appearance.
2. Foreign body aspiration: may be detected on X-ray or by bronchoscopy.
3. Cystic fibrosis: sweat test is definitive diagnostic test.
4. Asthma: pattern of symptoms, absence of fever; inspiratory wheezing; prolonged expiratory phase.
5. Aspiration: swallowing study to determine silent or free aspiration.
6. Tracheoesophageal fistula: gas-filled bowel on X-ray in an infant with respiratory problems and drooling at birth.
7. Bronchiolitis: rapid testing for viral antigen.
8. Right lower lobe pneumonia can present as GI process; X-ray can differentiate.
9. Right upper lobe pneumonia can present as meningitis, severity of illness, lumbar puncture.
G. Treatment.
1. Viral pneumonia.
a. Supportive care; typically mild illness and can be managed at home; young infant at risk for respiratory fatigue and more severe symptoms.
2. Bacterial pneumonia.
a. Dependent on bacteria; dependent on condition of child (oxygenation, hydration status, age: infants younger than 4-6 months are usually hospitalized).
b. Acetaminophen for fever and chest pain.
c. Antibiotic treatment is generally 7-10 days.
d. Amoxicillin is outpatient drug of choice; alternative choices are clarithromycin for children 6 weeks to 4 years of age; erythromycin for children older than 4 years of age.
e. With high level of penicillin-resistant pneumococci present in community, consider cefuroxime, amoxicillin-clavulanate (Augmentin), or azithromycin.
3.
M. pneumoniae.
a. Usually mild disease that can be managed at home.
b. Erythromycin is drug of choice.
c. Antibiotic treatment is generally 7-10 days.
d. Acetaminophen for fever.
H. Follow up.
1. Follow-up X-ray not needed in most cases of community-acquired pneumonia.
a. Exceptions include severe illness requiring hospitalization, complications such as abscess, empyema, pleural effusion.
b. May take up to 6 weeks for significant improvement.
2. Daily contact with healthcare provider may be indicated with more serious illness, in children with underlying conditions, and in very young children.
3. Recheck child if no improvement after 48 hours of treatment or if worsening occurs.
4. Follow-up visit at 10-14 days; occasional relapse may occur.
I. Complications.
| Empyema, 510.9 | Pleural effusion, 511.9 |
| Encephalopathy, 248.3 | Pulmonary abscess, 513 |
| Guillain-Barré syndrome, 357 | Staphylococcus aureus, 041.11 |
| Meningoencephalitis, 323.9 | Stevens-Johnson syndrome, 695.1 |
| Mycoplasma pneumoniae , 483 | Toxic shock syndrome, 040.82 |
| Pericarditis, 423.9 | Transverse myelitis, 323.9 |
1. Severe disease requiring hospitalization and ventilatory support.
2. Empyema, pulmonary abscess, pleural effusion, pericarditis.
3.
S. aureus:
toxic shock syndrome.
4.
M. pneumoniae:
Stevens-Johnson syndrome, transverse myelitis, meningoencephalitis, encephalopathy, Guillain-Barré syndrome.
J. Education.
1. Immunizations are essential to decrease individual morbidity and mortality associated with pneumonia but also to reduce incidence in community.
2. Understand symptoms that warrant immediate attention (lethargy, seizure, severe respiratory distress) and symptoms that require follow up (no improvement 48 hours after starting antibiotics, worsening of respiratory symptoms, signs of dehydration).
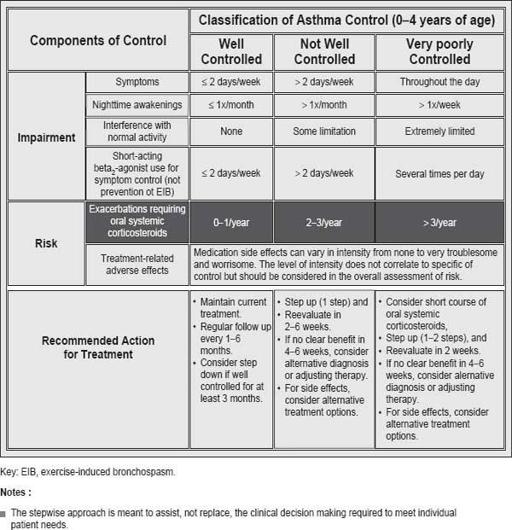
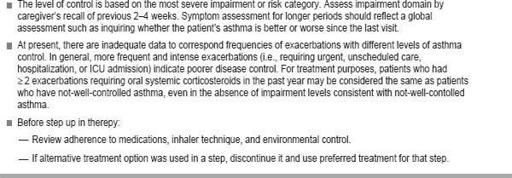
Figure 24-1
Assessing asthma control and adjusting therapy in children 0-4 years of age.
3. Need to give antibiotic as prescribed for full course.
Other books
Twin Dragons: Dragon Lords of Valdier Book 7 by S. E. Smith
Annie's Anal Adventure (Snowed In, #1) by M.R. Johnson
The Millionaire's Secret Wish by Leanne Banks
Altered by Gennifer Albin
Honky Tonk Samurai (Hap and Leonard) by Joe R. Lansdale
The Secrets of Rosa Lee by Jodi Thomas
Mr Gum and the Secret Hideout by Andy Stanton
The Debt 8 (Club Alpha) by Kelly Favor
The Incorporated Knight by L. Sprague de Camp, Catherine Crook de Camp