The Lupus Book: A Guide for Patients and Their Families, Third Edition (15 page)
Read The Lupus Book: A Guide for Patients and Their Families, Third Edition Online
Authors: Daniel J. Wallace

other process is being missed and also to confirm the anatomy of the area
involved.
Joints and Soft Tissues Often Involved in Lupus
Any joint lined with synovium may be affected by systemic lupus. Starting at
the top, the
temporomandibular joint
(TMJ or jaw joint) can produce symptoms
Why the Aches? Arthritis, Muscles, and Bone
[81]
in up to one-third of lupus patients. Manifesting itself as jaw pain, TMJ inflammation is often confused with
myofascial pain
(a regional form of fibrositis), which consists of tense facial muscles.
Fibromyalgia
(see the next section) affects 20 percent of lupus patients.
The upper
cervical spine
is the only part of the spinal column lined with enough synovium to produce significant inflammation. Inflammation of this area
in lupus patients is usually mild and produces pain in the back of the head.
Patients who have been treated with steroids for many years can develop insta-
bility in the ligaments supporting the neck, so I may recommend that these
patients use a collar when driving a car. Again, myofascial problems in the neck and upper back area are much more common than synovitis of the upper cervical
spine. Myofascial pain is managed with heat, traction, cervical pillows, muscle relaxants, pain killers, and remedies that improve sleep habits.
Shoulder
inflammation is not uncommon in lupus patients and often, when arms are raised over the head, feels the way a ‘‘bursitis’’ pain does. Such inflammation responds to anti-inflammatory medications or a local injection.
Elbows
are occasionally affected in lupus patients. About 10 percent of patients may have
rheumatoid-like nodules
in this area, which feel like little peas.
These nodules are much smaller than those seen in rheumatoid arthritis and are
of little clinical importance except that they may cause the area below the elbow to fill up with fluid when they break down.
The
hands and wrists
are affected in most lupus patients, with swelling occurring in up to 50 percent of those with systemic lupus. Symptoms of stiffness and aching are frequently experienced in the morning hours. Since it is used
more often, the dominant hand is usually more inflamed. In other words, because most people are right-handed, the knuckles of the right hand are larger than
those in the left. With chronic inflammation, an ‘‘ulnar drift’’ or outward movement of the knuckles away from the body is observed. Inflammation of the
tendons of the hand may result in
trigger fingers
(locking) or deformities in the form of contractures (shortening of the tendon) or tendon ruptures.
Carpal tunnel
syndrome
has received a lot of attention in the media as a result of ‘‘repetitive strain syndrome,’’ suffered by certain workers such as machine and computer
operators. In lupus, it results from chronic swelling in the wrist, which com-
presses the nerves running through the wrist to the hand. Occasionally, the soft tissues show evidence of
calcinosis
, or calcium deposits under the skin. More commonly seen in scleroderma than systemic lupus, these deposits may cause
occasional pain or may break through the skin, ooze, and drain.
Costochondral margin
irritation, or
costochondritis
, produces chest pain that may mimic a heart attack. The costochondral margin is defined as the place
where the sternum (breastbone) meets the ribs. Also known as
Tietze’s syn-
drome
, costochondritis is frequently observed in lupus but is also found in many healthy young women.
Even though the lower spine is not involved in lupus, some of my patients
[82]
Where and How Can the Body Be Affected by Lupus?
complain of back pain, since their
hips and sacroiliac
joints are lined with synovium. About one-third complain of discomfort in this area, but destructive
changes are unusual.
Knee
pain, on the other hand, is quite common in lupus patients, but since most lupus patients are young, internal damage to the knee
as a consequence of athletic endeavors must also be ruled out.
The
ankle and feet
are common focuses of joint involvement. Ankles can be swollen because of fluid retention, poor circulation, or proteins that have leaked from the kidneys. In addition, swelling can occur from direct joint inflammation or altered gait as a result of foot abnormalities or deformities. Metatarsals are the foot bones in our soles that bear the brunt of our weight when we walk. In
systemic lupus, the supporting ligaments of the toes loosen and produce bunions and calluses. This may evolve to the point where patients must walk on their
metatarsal heads (a normally straight bone), often causing severe foot pain. If the problem is determined to be a local one, I prescribe anti-inflammatory agents and special footwear. Local injections may be used, and occasionally surgery is necessary.
THE MUSCLES IN LUPUS PATIENTS
Two-thirds of my lupus patients complain of muscle aches, which are called
myalgias
. Most frequently located in the muscles between the elbow and neck and the knee and hip, myalgias are rarely associated with weakness. Inflammation of the muscles, or
myositis
, is observed in 15 percent of patients with systemic lupus. Established by blood elevations of the muscle enzyme CPK
(creatine phosphokinase), a diagnosis of myositis necessitates steroid therapy, because muscle inflammation may cause permanent muscle weakness and atrophy if not treated. Occasionally, an electromyogram (EMG) or ‘‘cardiogram’’
of the muscles is needed to confirm the presence of an inflammatory process.
Muscle biopsies are rarely necessary. In addition to physical inactivity, another cause of muscle weakness (not pain) is chronic, long-term steroid use for inflammation, which paradoxically induces muscle atrophy and wasting. In rare
cases, high doses of antimalarial agents can cause muscle weakness.
A number of my lupus patients have aching muscles in the neck and upper
back areas as well as tenderness in the buttocks, but these aches do not respond to steroids or anti-inflammatories.
Fibromyalgia
consists of amplified pain in what are known as ‘‘tender points’’ (in areas we have already discussed, among
others). About 6 million Americans have fibromyalgia. Associated with trauma,
infections, and inflammation, patients with fibromyalgia complain of fatigue,
sleep disorders, skin that is painful to the touch, aggravation by stress, and a relatively poor response to physical therapy. Lowering steroid doses can also
temporarily aggravate fibromyalgia (‘‘steroid withdrawal syndrome’’). I manage
fibromyalgia with tricyclic antidepressants—which can relax muscles, induce
restful sleep, and raise pain thresholds—along with other non-anti-inflammatory
Why the Aches? Arthritis, Muscles, and Bone
[83]
interventions. It can be difficult to differentiate lupus flareups from aggravated fibromyalgia. (See Chapter 23 for a complete discussion.)
BONES IN LUPUS PATIENTS
Osteoporosis
Osteoporosis
, or thinning of the bones as a result of lost calcium, may be observed in systemic lupus. A complete discussion of this disease is found in
Chapter 29.
Avascular Necrosis
Penelope went to her doctor with a sudden onset of severe pain in her right
hip. She had a 5-year history of lupus, which involved her skin and joints,
and had experienced recurrent bouts of pleural effusions (fluid in her lungs).
Her disease was well controlled with 20 milligrams of prednisone a day.
An x-ray of her hip was normal, but since Penelope rarely complained, Dr.
Smith ordered an MRI (magnetic resonance imaging) scan, which revealed
avascular necrosis (defined below). The pain did not respond to any anti-
inflammatory medications and only an aspirin with codeine preparation
provided temporary relief. Dr. Smith referred Penelope to an orthopedist
who put in an artificial hip joint. She is feeling fine now.
One of the most feared consequences of steroid therapy in lupus patients is
a condition known as
avascular
(or
aseptic) necrosis
. Experienced as a localized pain, avascular necrosis begins when fat clots produced by steroids clog up the blood supply to bone and deprive it of oxygen. This results in dead bone tissue, which, in turn, produces a tremendous amount of pain and ultimately the destruction of bone. About 10 percent of avascular necrosis is not the result of
steroids but derives from clots in the blood supply to the bone in patients with the circulating lupus anticoagulant or in those with active inflammation of blood vessels (vasculitis), which obstructs blood flow to the bone. Even though avascular necrosis is seen in 5 to 10 percent of those with systemic lupus, signs of the affliction may not appear on plain x-rays for many months. Early cases may
be identified by MRI. The most common target areas are the hip, shoulder, and
knee. Crutches may be helpful and medications may alleviate symptoms some-
what. Limited surgical procedures including revascularization grafts or core decompression are beneficial if performed early in selected joints, but the over-
whelming majority of patients ultimately require surgery for joint replacement.
Summing Up
Most lupus patients complain of joint aches, but only a minority demonstrate
inflammatory arthritis and only 10 percent develop deformities. Inflamed syn-
[84]
Where and How Can the Body Be Affected by Lupus?
ovium can cause pain and swelling in joints, tendons, and bursae. The small
joints of the hands and feet are most frequently involved. Muscles aches are
also present in most patients with systemic lupus, but inflammatory muscle dis-
ease (myositis) is observed in only 15 percent during the course of their disease.
In order to provide optimal management, arthritis, myalgias, and myositis due
to lupus must be differentiated from avascular necrosis, fibromyalgia, and the
adverse effects of lupus medications.
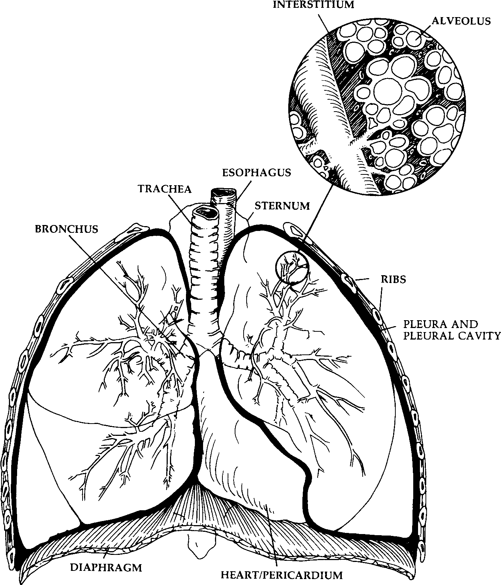
Every grammar school child learns that the heart and lungs are the heart of the engine that runs the human body. If you suffer from chest pains or notice shortness of breath, you are reminded of the importance of these two organs. And
for those of us treating lupus patients, studying the effect of systemic lupus on the heart and lungs is critical. Most lupus patients have complaints pertaining to the chest. This chapter will review the pulmonary and cardiac manifestations of lupus. Figures 14.1 and 14.2 depict the principal anatomic areas in the lungs and heart that are relevant to our discussion.
THE LUNGS
When the lungs are working perfectly, they exchange oxygen for carbon dioxide
effortlessly. When lupus affects the lungs, or pulmonary system, as many as
eight different problems can arise that impede the ability to breathe easily. Doctors can diagnose such problems fairly accurately and quickly by using a variety of tests, including chest x-rays, pulmonary function tests, lung scans, heart ultrasounds, biopsies, drainage of lung fluid, and analysis of lung cells derived through bronchoscopy.
The Pulmonary Workup
Surprisingly, patients may not think of mentioning their lung complaints during an interview. I make a point of asking about shortness of breath, chest pains,
pain on taking a deep breath, dry cough, coughing up blood, fever, and rapid
breathing. I also inquire about tobacco use and take a job history to see if there has been exposure to toxins. For example, contact with coal or asbestos can
certainly damage the lungs.
In addition to a physician listening to the patient’s lung, the first diagnostic tool used in evaluation is the
chest x-ray
. It is inexpensive, quick, widely avail-
[86]
Where and How Can the Body Be Affected by Lupus?
Fig. 14.1.
The Lung
able, and can detect nearly all the important syndromes discussed in this chapter.
Should additional testing be necessary, a
CT
(computed tomography)
scan
or
MRI
may demonstrate structural abnormalities in the chest cavity and pleura.
(The CT scan is a modified x-ray, whereas the MRI scanner uses magnets to
create an image and releases no radiation.)
Ultrasound
machines employ sound waves to create an image and are used to evaluate pleural disorders. Measurement of
arterial blood gases
(taking blood from the artery instead of a vein) demonstrates how much oxygen is flowing through a patient’s arteries, and
pulse
oximetry
is a simple, noninvasive measurement of how well the body is satu-Pants and Pulses: The Lungs and Heart