Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (125 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

PANCREATITIS
PANCREATITIS, ACUTE
Laboratory Findings
Lipase
:
Serum lipase increases within 3–6 hours with peak at 24 hours and usually returns to normal over a period of 8–14 days; is superior to amylase; increases to a greater extent and may remain elevated for up to 14 days after amylase returns to normal. In patients with signs of acute pancreatitis, pancreatitis is highly likely (clinical specificity = 85%) when lipase ≥5× upper reference limit (URL); if values change significantly with time, and if amylase and lipase changes are concordant. (
Lipase should always be determined whenever amylase is determined.
) Urinary lipase is not clinically useful. It has been suggested that a lipase:amylase ratio >3 (and especially >5) indicates alcoholic rather than nonalcoholic pancreatitis. If lipase ≥5× URL, acute pancreatitis or organ rejection is highly likely but unlikely if <3× URL (Figure
5-1
).
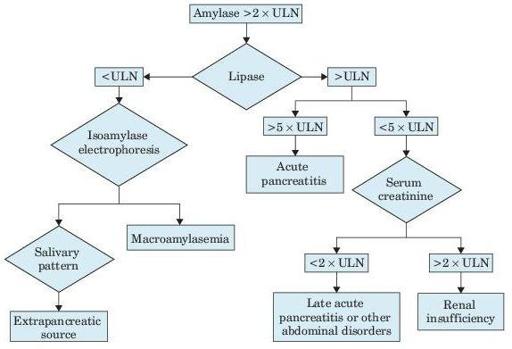
Figure 5–1
Algorithm for increased serum amylase and lipase. ULN, upper limit of normal.
Amylase
: Increase begins in 3–6 hours, rises rapidly within 8 hours in 75% of patients, reaches maximum in 20–30 hours, and may persist for 48–72 hours; >95% sensitivity during the first 12–24 hours. The increase may be ≤40× normal, but the height of the increase and rate of fall do not correlate with the severity of the disease, prognosis, or rate of resolution. In patients with signs of acute pancreatitis, amylase >3× ULN or >600 Somogyi units/dL is very suggestive of acute pancreatitis. An increase >7–10 days suggests an associated cancer of the pancreas or pseudocyst, pancreatic ascites, or nonpancreatic etiology. Similar high values may occur in obstruction of the pancreatic duct; they tend to fall after several days; ≤19% of patients with acute pancreatitis (especially when seen more than 2 days after onset of symptoms) may have normal values, especially with an alcoholic etiology and longer duration of symptoms, even when dying of acute pancreatitis. May also be normal in relapsing chronic pancreatitis and patients with hypertriglyceridemia (technical interference with test). Frequently normal in acute alcoholic pancreatitis. Acute abdomen due to GI infarction or perforation rather than acute pancreatitis is suggested by only moderate increase in serum amylase and lipase (<3× URL), evidence of bacteremia. Of patients with acute alcoholic intoxication, 10–40% have elevated serum amylase (about half are salivary type); they often present with abdominal pain, but increased serum amylase is usually <3× URL. Levels >25× URL indicate metastatic tumor rather than pancreatitis. Serum pancreatic isoamylase can distinguish elevations due to salivary amylase that may account for 25% of all elevated values. (In healthy persons, 40% of total serum amylase is pancreatic type and 60% is salivary type.) Only slight increase in serum amylase and lipase values suggests a different diagnosis than acute pancreatitis.
Many drugs increase both amylase and lipase in serum.
Increased urinary amylase tends to reflect serum changes by a time lag of 6–10 hours, but sometimes, increased urine levels are higher and of longer duration than serum levels. The 24-hour level may be normal even when some of the 1-hour specimens show increased values. Amylase levels in hourly samples of urine may be useful. Ratio of amylase clearance to creatinine clearance is increased (>5%) and avoids the problem of timed urine specimens; also increased in any condition that decreases tubular reabsorption of amylase (e.g., severe burns, DKA, chronic renal insufficiency, multiple myeloma, acute duodenal perforation). Considered not specific and now discouraged by some but still recommended by others.
Calcium
: Serum level is decreased in severe cases 1–9 days after onset (due to binding to soaps in fat necrosis). The decrease usually occurs after amylase and lipase levels have become normal. Tetany may occur. (
Rule out hyperparathyroidism if serum calcium is high or fails to fall in hyperamylasemia of acute pancreatitis.
)
Bilirubin
: Serum levels may be increased when pancreatitis is of biliary tract origin but is usually normal in alcoholic pancreatitis. Serum ALP, ALT, and AST may increase and parallel serum bilirubin rather than amylase, lipase, or calcium levels. Marked amylase increase (e.g., >2,000 U/L) also favors biliary tract origin. Fluctuation >50% in 24 hours of serum bilirubin, ALP, ALT, and AST suggests intermittent biliary obstruction.
Trypsin
: Serum level is increased. High sensitivity makes a normal value useful for excluding acute pancreatitis. But low specificity (increased in large proportion of patients with hepatobiliary, bowel, and other diseases and renal insufficiency; increased in 13% of patients with chronic pancreatitis, 50% with pancreatic carcinoma) and RIA technology limit utility.
CRP
: Level peaks 3 days after onset of pain; at 48 hours, sensitivity = 65–100%, PPV = 37–77%. Level of 150 mg/L distinguishes mild from severe disease.
Laboratory criteria for severe disease or predictor of mortality
:
PaO
2
<60 μmol/L
Creatinine >2 mg/dL after rehydration
Blood glucose >250 mg/dL
Hemoconcentration (Hct >47% or failure to decrease in 24 hours after admission), but Hct may be decreased in severe hemorrhagic pancreatitis
GI bleed >500 mL/24 hours
Presence, volume, and color of peritoneal fluid
Methemalbumin may be increased in serum and ascitic fluid (AF) in hemorrhagic (severe) but not edematous (mild) pancreatitis; may distinguish these two conditions but not useful in diagnosis of acute pancreatitis.