Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (175 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

BOOK: Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis
13.99Mb size Format: txt, pdf, ePub

Total protein
: Usually normal or decreased. Serum albumin parallels functional status of parenchymal cells and may be useful for following progress of liver disease, but it may be normal in the presence of considerable liver cell damage. Decreasing serum albumin may reflect development of ascites or hemorrhage. Serum globulin level is usually increased; it reflects inflammation and parallels the severity of the inflammation. Increased serum globulin (is usually gamma) may cause increased total protein, especially in chronic viral hepatitis and post–hepatitic cirrhosis.

Total cholesterol
: Normal or decreased. Progressive decrease in cholesterol, HDL, LDL with increasing severity. Decrease is more marked than in chronic active hepatitis. LDL may be useful for prognosis and selecting patients for transplantation. Decreased esters reflect more severe parenchymal cell damage.

Other core laboratory findings
: BUN is often decreased (<10 mg/dL); increased with GI hemorrhage. Serum uric acid is often increased. Electrolytes and acid–base balance are often abnormal and reflect various combinations of circumstances at the time, such as malnutrition, dehydration, hemorrhage, metabolic acidosis, respiratory alkalosis. In cirrhosis with ascites, the kidney retains increased sodium and excessive water, causing dilutional hyponatremia. Increased blood ammonia in liver coma and cirrhosis and with portacaval shunting of blood.

Hematology
: WBC is usually normal with active cirrhosis; increased (<50,000/μL) with massive necrosis, hemorrhage, and so on; decreased with hypersplenism. Anemia reflects increased plasma volume and some increased destruction of RBCs. If more severe, rule out hemorrhage in the GI tract, folic acid deficiency, and excessive hemolysis.
CSF findings
: CSF is normal except for increased glutamine levels, which reflect brain ammonia levels (due to conversion from ammonia). Glutamine >35 mg/ dL is always associated with hepatic encephalopathy (normal = 20 mg/dL); correlates with depth of coma and is more sensitive than arterial ammonia.
Considerations
See Tables 5-7 and 5-8.
Laboratory findings due to complications or sequelae, often in combination.
Abnormalities of coagulation mechanisms (see Chapter
10
, Hematologic Disorders) such as prolonged PT (does not respond to parenteral vitamin K as frequently as in patients with obstructive jaundice). Prolonged bleeding time in 40% of cases due to decreased platelets and/or fibrinogen.
Hepatic encephalopathy (neurologic and mental abnormalities in some patients with liver failure or portosystemic shunt). Diagnosis is clinical; characteristic laboratory findings are supportive but not specific.
See Table
5-9
.
Markers that may indicate progression to cirrhosis include decreased albumin; increased globulins; AST/ALT ratio >1; increased bilirubin, mainly unconjugated; increased PT; and decreased platelet count.
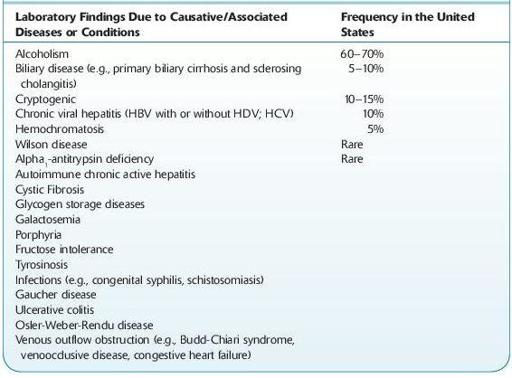
TABLE 5–7. Causes of Liver Disease with Associated Conditions
Other books
A Little Night Muse by Slade, Jessa
This Beautiful Thing (Young Love Series) by Heath, Amanda
Famous Last Meals by Richard Cumyn
Horseman of the Shadows by Bradford Scott
Subject Nightingale 1: Birth and Death by Tim Cody
Fallen Angel of Mine by John Corwin
Americans in Paris: Life & Death Under Nazi Occupation by Charles Glass
Board Stiff: A Dead-End Job Mystery by Viets, Elaine
Like Never Before by Melissa Tagg
Outbreak! Plagues That Changed History by Barnard, Bryn