Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (227 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

5. Low blood urea nitrogen (BUN) and serum uric acid concentration
6. Relatively normal serum creatinine concentration
7. Normal acid–base and potassium balance
8. Causes such as adrenal insufficiency and hypothyroidism need to be identified since the associated SIADH can be corrected by hormone replacement.
9. Currently, measurement of plasma ADH levels has very limited role in the diagnosis of SIADH. There are several reasons for this. First, the elevated plasma ADH levels seen in SIADH generally remain within normal reference range and are abnormal only in relation to plasma osmolality. Second, the current assays for ADH cannot detect elevations in 10–20% of patients with SIADH. Third, most disorders of volume depletion are associated with elevation of plasma ADH levels and thus cannot be distinguished.
Suggested Readings
Kronenberg HM, Melmed S, Polonsky KS, et al.
Williams Textbook of Endocrinology
, 11th ed. Philadelphia, PA: Saunders, Elsevier Inc.; 2008.
Rose BD. Pathophysiology and etiology of the syndrome of inappropriate antidiuretic hormone secretion (SIADH). In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Sterns RH. Evaluation of the patient with hyponatremia. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
DISORDERS OF THE PARATHYROID GLAND AND MINERAL METABOLISM
HYPERPARATHYROIDISM
Definition
Primary hyperparathyroidism is autonomous hypersecretion of parathyroid hormone (PTH) from the parathyroid glands. Secondary hyperparathyroidism occurs in patients with chronic advanced renal disease that causes retention of phosphate, inadequate vitamin D activation, chronic low serum calcium, and therefore compensatory hyperplasia of the parathyroid glands with compensatory secretion of PTH. This Chapter focuses solely on primary hyperparathyroidism.
Overview
Primary hyperparathyroidism is frequently identified in asymptomatic patients with an elevated serum calcium concentration. It is estimated to have a prevalence of 1 case per 1,000 people. Primary hyperparathyroidism can occur at any age, but the majority of cases occur in patients >45 years of age.
Common Causes
Primary hyperparathyroidism can usually be differentiated from other causes of hypercalcemia by the demonstration of an elevated serum PTH concentration.
1. Parathyroid adenoma is the most common cause of hyperparathyroidism and accounts for approximately 90% of the cases. Most patients have a single enlarged gland with a single adenoma. The remaining glands are usually normal.
2. Parathyroid hyperplasia accounts for approximately 6% of the cases. It involves all four glands and can occur either as isolated or as part of a syndrome such as MEN type 1 or 2 or familial hyperparathyroidism.
3. Parathyroid carcinoma is a rare cause of hyperparathyroidism and constitutes 1–2% of the cases. The diagnosis of carcinoma requires demonstration of local invasion of contiguous structure, metastases to lymph node, or distant metastases.
4. Familial hypocalciuric hypercalcemia is caused by an inactivating mutation in the calcium-sensing receptor in the parathyroid glands and the kidneys. It is characterized by a family history of hypercalcemia, a young age of onset, lack of symptoms or complications, and specifically by a low urine calcium excretion with calcium/creatinine (Ca/Cr) clearance ratio <0.01 in 90% of patients. These patients have normal or only very slightly elevated PTH concentrations.
Who Should Be Suspected?
Primary hyperparathyroidism should be suspected in patients with
1. Elevated serum calcium levels, especially when it persists for years
2. Nephrolithiasis
3. Metabolic acidosis
4. Unexplained osteoporosis, bone pain, and pathologic fractures
5. Osteitis fibrosa cystica, which is characterized by subperiosteal bone resorption on the radial aspect of middle phalanges, tapering of distal clavicles, “salt and pepper” appearance of the skull, bone cysts, and brown tumors of the long bones
Laboratory Findings
The diagnosis of primary hyperparathyroidism depends on demonstrating elevated serum calcium in the presence of increased PTH (Figure
6-13
).
1. Measurement of serum calcium. A single elevated serum calcium concentration should be repeated to confirm the presence of hypercalcemia. Both total and ionized calcium concentrations should be obtained. The patient’s oral calcium and vitamin D supplements should be withheld before the workup.
2. Measurement of PTH. Approximately 80–90% of patients with primary hyper-parathyroidism have elevated PTH. In the remaining patients, normal or only minimally elevated PTH is detected, but these values are inappropriately high in the setting of an elevated serum calcium level. In patients with non–PTH-mediated hypercalcemia, intact PTH is <25 pg/mL. Parathyroid hormone–related protein (PTHrP), which is the humoral cause of cancer-related hypercalcemia, is not detected in the intact PTH assay.
3. Urinary calcium excretion. A 24-hour urine calcium quantitation should be measured if familial hypocalciuric hypercalcemia is suspected. The finding of 24-hour urine calcium excretion <100 mg and Ca/Cr clearance ratio <0.01 confirms the diagnosis.
4. Patients who have a familial history of hyperparathyroidism or those suspected of having hyperparathyroidism in the context of MEN syndromes should also be evaluated for associated disorders, particularly for pheochromocytoma and thyroid medullary carcinoma.
5. Vitamin D metabolites. Patients with primary hyperparathyroidism convert more calcidiol to calcitriol than normal individuals. Therefore, serum concentrations of
1
,
25-dihydroxyvitamin D
3
(calcitriol) may be at upper limits of normal or elevated. However, an elevated value is not specific, and thus the measurement of
1,25-dihydroxyvitamin D
3
(calcitriol) is not generally needed to confirm the diagnosis. However, it is helpful to differentiate from the cases with an isolated PTH increase in the absence of hypercalcemia due to vitamin D deficiency.
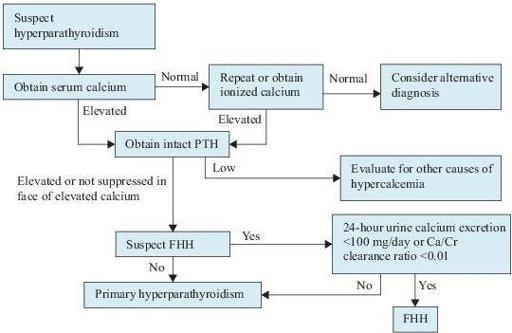
Figure 6–13
Algorithm for the workup of hyperparathyroidism. Ca/Cr, calcium/creatinine; FHH, familial hypocalciuric calcemia; PTH, parathyroid hormone.