Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (225 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

C. Neurologic symptoms.
a. Visual defects. Impaired vision is the most common symptom that leads a patient with a nonfunctioning adenoma to seek medical attention. Visual impairment is caused by suprasellar extension of the adenoma, leading to compression of the optic chiasm. The most common complaint is diminished vision in the temporal fields (bitemporal hemianopsia).
b. Headaches
c. Diplopia
II. Signs
A. Pituitary apoplexy. Sudden hemorrhage into the adenoma can cause excruciating headache and diplopia. It usually occurs spontaneously but occasionally is precipitated by administration of an anticoagulant.
B. Pituitary incidentaloma. Pituitary masses discovered incidentally on imaging studies are further evaluated based on their sizes. Incidental microadenomas refer to masses <10 mm in diameter. Patients with microadenomas should be evaluated clinically for hormonal hypersecretion and chemically for any hypersecretion suspected clinically. Serum prolactin level should be measured if there is no clinical suspicion of hormonal hypersecretion. When a macroadenoma (≥10 mm in diameter) is identified, evidence for hormonal excess should be sought and assessment of overall pituitary function and formal visual fields is required.
Laboratory Findings (Figure
6-12
)
1. A serum prolactin of >200 ng/mL almost always indicates a prolactinoma, although other causes should be considered, such as pregnancy, lactation, stress, dopamine receptor antagonists (e.g., neuroleptics, metoclopramide), primary hypothyroidism, and renal failure. Concentrations between 20 and 200 ng/mL could be due to a lactotroph adenoma or to any other sellar mass. The finding of a large tumor with only minimally elevated prolactin indicates that the tumor is not a prolactinoma but is causing pituitary stalk compression and loss of dopamine inhibition of prolactin secretion.
2. The best test for the diagnosis of acromegaly and growth hormone–secreting tumors is measurement of serum insulin-like growth factor I (IGF-I). IGF-I levels need to be corrected for age and sex. Among patients with equivocal values, serum growth hormone secretion after oral glucose administration can be obtained. Random growth hormone measurements are not reliable, since growth hormone is secreted episodically and may be elevated with anxiety, exercise, acute illness, chronic renal failure, and diabetes.
3. Twenty-four–hour urine free cortisol quantification or midnight salivary cortisol test for Cushing disease
4. LH, FSH, with testosterone in male patients or estradiol in female patients
5. TSH and free T
4
for thyroid function assessment
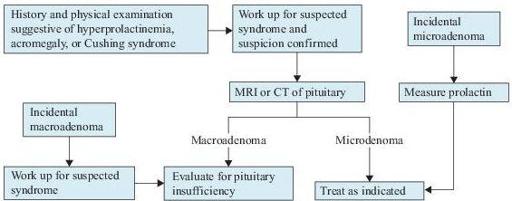
Figure 6-12
Pituitary tumor algorithm. CT, computed tomography; MRI, magnetic resonance imaging.
Suggested Readings
Khan F, Sachs H, Pechet L, et al.
Guide to Diagnostic Testing
. Philadelphia, PA: Lippincott Williams & Wilkins; 2002.
Kronenberg HM, Melmed S, Polonsky KS, et al.
Williams Textbook of Endocrinology
, 11th ed. Philadelphia, PA: Saunders, Elsevier Inc.; 2008.
Snyder PJ. Causes, presentation and evaluation of sellar masses. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Snyder PJ. Clinical manifestations and diagnosis of gonadotroph and other clinically nonfunctioning adenomas. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Snyder PJ. Pituitary incidentaloma. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
DIABETES INSIPIDUS
Definition
Diabetes insipidus (DI) is a disorder characterized by excretion of a large volume of dilute hypotonic urine.
Common Causes
1. Central DI is caused by inability to synthesize or secrete vasopressin [antidiuretic hormone (ADH)] in the neurohypophyseal system. In complete central DI, ADH levels are undetectable and polyuria is severe. In partial central DI, ADH levels are subnormal but detectable, and polyuria is less extreme. The most common causes of central DI include the following:
a. Idiopathic disease. It has been suggested that autoimmune destruction to the ADH-producing cells is involved in many patients.
b. Familial and congenital disorders
c. Primary or secondary tumors. Most often due to primary suprasellar and intrasellar tumors including craniopharyngiomas and germinomas, metastatic carcinomas (lung, breast), leukemias, and lymphomas.
d. Infiltrative disorders. Patients with Langerhans cell histiocytosis are at particularly high risk for central DI. Other infiltrative disorders include granulomatous lesions such as sarcoidosis, tuberculosis, syphilis, and Wegener granulomatosis.
e. Neurosurgery or trauma
f. Hypoxic encephalopathy
g. Post–supraventricular tachycardia
h. Anorexia nervosa
2. Nephrogenic DI is characterized by renal resistance to the action of ADH, leading to a decrease in urinary concentrating ability. The most common causes of nephrogenic DI include
a. Chronic renal failure seen in chronic pyelonephritis, analgesic nephropathy, or nephrosclerosis
b. Other tubulointerstitial diseases such as polycystic kidney disease, medullary cystic kidney disease, sickle cell disease or trait, renal amyloidosis, and Sjögren syndrome
c. Release of bilateral urinary tract obstruction
d. Drugs such as lithium, cidofovir, foscarnet, vasopressin V2 receptor antagonists, amphotericin B, demeclocycline, ifosfamide, ofloxacin, orlistat, and didanosine
e. Pregnancy
f. Hereditary renal tubular unresponsiveness to vasopressin due to genetic mutations in the vasopressin V2 receptor gene or aquaporin-2 gene
g. Prolonged potassium depletion and hypokalemia (condition is reversed by restoring potassium level to normal)
h. Prolonged hypercalciuria, usually with hypercalcemia (condition is reversed by restoring calcium level to normal)
3. Primary polydipsia is characterized by a primary increase in water intake. It can be due to
a. Psychogenic illnesses
b. Hypothalamic lesions affecting thirst center
c. Drugs (such as thioridazine, chlorpromazine, anticholinergic agents) causing dry mouth and leading to increased thirst
Who Should Be Suspected?
The main clinical manifestation of DI is polyuria. Polyuria is defined as urine volume exceeding 3 L/day in adults and 2 L/m
2
in children. It must be differentiated from other similar urinary complaints such as urinary frequency, nocturia, urgency, and urinary incontinence, which are not associated with an increase in the total urine output.
The cause of polyuria is often suggested from the history such as age of onset. In the majority of hereditary nephrogenic DI, severe polyuria manifests during the first week of life. In familial central DI, polyuria may present after the first year of life, sometimes in young adulthood. In adults, the onset of polyuria is usually abrupt in central DI and almost always gradual in acquired nephrogenic DI or primary polydipsia. The new onset of nocturia in the absence of other causes of nocturia (e.g., prostatic enlargement in men over 50 years of age or urinary tract infection in children) is often a first clue to DI. Family history of polyuria suggests the familial forms of both central and nephrogenic DI.