Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (792 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

BOOK: Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis
10.63Mb size Format: txt, pdf, ePub
CARDIOVASCULAR DRUGS (SEE DIGOXIN)
*
Definition
Cardiovascular drugs include the antiarrhythmics, the anticoagulant warfarin, and antihypertensives, as well as the β-adrenergic antagonist propranolol and the drug digoxin (see p. 925).

Normal therapeutic values:
see Table 16.15.
TABLE 16–15. Cardiovascular Drugs
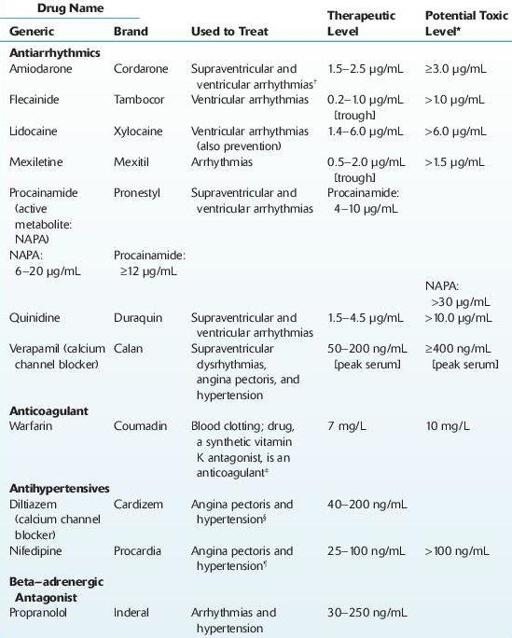
*Toxic concentrations have not been established.
† Monitor TSH and T
4
values during therapy.
‡ Prothrombin time is used to assess efficacy as target INR: 2.0–3.0. Consider long-term, low-intensity (INR 1.5–2.0),
or standard-intensity (INR 2–3) warfarin therapy for patients with idiopathic events.
§ Effect on platelets may increase bleeding time.
¶ Decreased glucose tolerance.
Use
To treat arrhythmia, hypertension, blood clotting, and angina.
The majority of these drugs are not routinely monitored as clinical effects do not generally correlate with serum or plasma levels. Notable exceptions are digoxin and procainamide.
Where concentrations are required, specific gas chromatography and HPLC procedures have been developed (e.g., procainamide/
N
-acetylprocainamide [NAPA], quinidine, mexiletine, diltiazem, verapamil, amiodarone, and metabolite, warfarin). Limits of quantitation vary according to the drug and methodology.
Immunoassay tests (e.g., FPIA) are available for procainamide, quinidine.
In addition, lidocaine, diltiazem, verapamil, and quinidine are qualitatively detectable in urine with a simple alkaline liquid–liquid or solid-phase extraction followed by GC/MS analysis. Limits of detection range from 50 to 250 ng/mL.
Interpretation
Rifampin may decrease verapamil serum concentrations.
Limitations
Other books
A McKettrick Christmas by Linda Lael Miller
Texas #4_Texas Christmas by R.J. Scott
The End of Never by Tammy Turner
Somewhere Only We Know ....... by Leanne Burn
The Billionaire's Embrace (The Silver Cross Club) by Bec Linder
Zombie Ocean (Book 2): The Lost by Grist, Michael John
The Visibles by Sara Shepard
Nieve by Terry Griggs
Sky Island by L. Frank Baum
1 The Bank of the River by Michael Richan