Fundamentals of Midwifery: A Textbook for Students (149 page)
Read Fundamentals of Midwifery: A Textbook for Students Online
Authors: Louise Lewis

BOOK: Fundamentals of Midwifery: A Textbook for Students
8.24Mb size Format: txt, pdf, ePub
347
OBSTETRIC EARLY WARNING CHART.
FOR MATERNITY USE ONLY
NAME:
DOB:
CHI: WARD:
Contact doctor for early intervention if patient triggers one red or two yellow scores at any one time
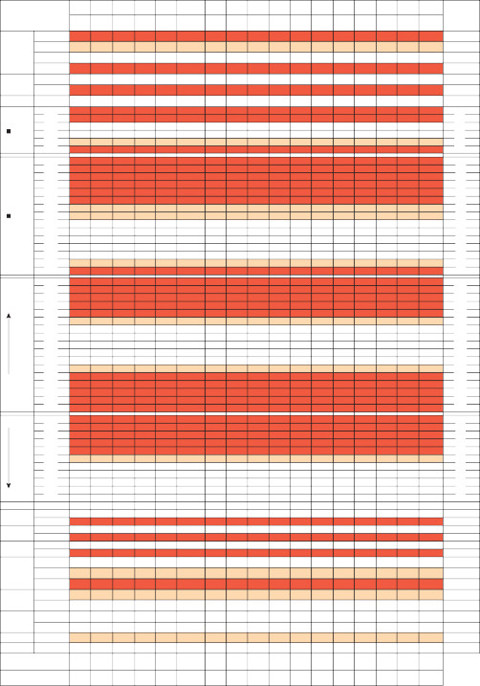
Date: Time:

Systolic blood pressure
348
RESP (write rate in corresp. box)
Temp
Saturations O2 Conc.
>30
21–30
11–20
0–10
90–100%
<90%
%
39
38
37
36
35
170
160
150
140
HEART RATE
130
120
110
100
90
80
70
60
50
40
200
190
180
170
160
150
140
130
120
110
100
90
80
70
60
50
>30
21–30
11–20
0–10
90–100%
<90%
%
39
38
37
36
35
170
160
150
140
130
120
110
100
90
80
70
60
50
40
200
190
180
170
160
150
140
130
120
110
100
90
80
70
60
50
Diastolic blood pressure
Passed Urine Lechia
Proteinuria Liquor
NEURO RESPONSE
(√)
Pain Scorre (no.)
Nausea (√)
Looks unwell Looks unwell
130
120
110
100
90
80
70
60
50
40
Y or N Normal Heavy/Foul 2+
> 2+
Clear/Pink Green
Alert
Voice Pain/
Unresponsive
2–3
0–1
Yes (√)
No (√)
Yes (√)
No (√)
130
120
110
100
90
80
70
60
50
40
Y or N Normal Heavy/Foul 2+
>2+
Clear/Pink Green
Alert
Voice Pain/
Unresponsive
2–3
0–1
Yes (√)
No (√)
Yes (√)
No (√)
Total Yellow Scores Total Red Scores
Figure 16.1
Modified Early Obstetric Warning Scoring System chart. Source: Reproduced with permission of NHS Forth Valley.
Box 16.1 Effective clinical assessment
Observation of general appearance noting any pallor, clamminess, lethargy or obvious discomfort.
Ask the woman about how she feels – ask open questions to allow her to say how and what sheis feeling rather than simply responding to focused closed questions.
Vital sign recordings and other observations such as blood loss, peripheral perfusion, oedema, and urinalysis.
Assessment should be informed by and linked to history and diagnosis but should also bethorough and holistic to avoid missing co-existing problems.
Accurate, contemporaneous record keeping.
Table 16.1
Signs and symptoms of shock
 Blood pressure
Blood pressure
Systolic blood pressure is lower than 90 mmHg. Initially however blood pressure may rise due to compensatory mechanisms such as increased cardiac rate and contractility, vasoconstriction and water and salt conservation by the kidneys. A normal blood pressure therefore does not necessarily mean the woman is not in Stage One shock.
Pulse
Weak and rapid even at rest.
Skin
Pale, cool and clammy due to vasoconstriction and stimulation by sympathetic nervous system which causes sweating.
Mental state
Altered mental state which may result in confusion, agitation and restlessness.
Urine output
Reduced (normal urine output ranges from 0.5–2 mL/h/kg body weight).
Thirst
Occurs due to loss of extracellular fluid.
Nausea
Due to impaired gastrointestinal blood flow as a result of vasoconstriction.
Blood pH
Low due to acidosis.349Assessment of the woman should follow the recognised standard of ABCDE (see Box 16.2) and urine output. If the baby is still in utero any assessment should also address fetal wellbeing.
Management of shock
The principles of treatment and management are:
Table 16.1
Signs and symptoms of shock
 Blood pressure
Blood pressureSystolic blood pressure is lower than 90 mmHg. Initially however blood pressure may rise due to compensatory mechanisms such as increased cardiac rate and contractility, vasoconstriction and water and salt conservation by the kidneys. A normal blood pressure therefore does not necessarily mean the woman is not in Stage One shock.
Pulse
Weak and rapid even at rest.
Skin
Pale, cool and clammy due to vasoconstriction and stimulation by sympathetic nervous system which causes sweating.
Mental state
Altered mental state which may result in confusion, agitation and restlessness.
Urine output
Reduced (normal urine output ranges from 0.5–2 mL/h/kg body weight).
Thirst
Occurs due to loss of extracellular fluid.
Nausea
Due to impaired gastrointestinal blood flow as a result of vasoconstriction.
Blood pH
Low due to acidosis.349Assessment of the woman should follow the recognised standard of ABCDE (see Box 16.2) and urine output. If the baby is still in utero any assessment should also address fetal wellbeing.
Management of shock
The principles of treatment and management are:
Treat the cause (for example; haemorrhage, pulmonary embolism, sepsis).
Maintain airway and give oxygen therapy.
Restore cardiac output and perfusion by fluid resuscitation and drugs.
Provide analgesia where required.The effectiveness of the management can be assessed by the stabilisation of vital signs, increased urinary output and improved mental state. Continued assessment and evaluation is essential and should continue after the woman is apparently stabilised. It is also important that,350
 Box 16.2 ABCDE assessment of the critically ill patient
Box 16.2 ABCDE assessment of the critically ill patient
A = AIRWAY
 Box 16.2 ABCDE assessment of the critically ill patient
Box 16.2 ABCDE assessment of the critically ill patientA = AIRWAY
Check airway is not obstructed if patient is unconscious
Give oxygen
B = BREATHING
B = BREATHING
Check rate, depth and sound of breathing
Note whether chest expansion is equal
Record oxygen saturation if possible
C = CIRCULATION
C = CIRCULATION
Observe for cyanosis (central or peripheral)
Heart rate
Capillary refill time
D = DISABILITY

D = DISABILITY

Conscious level
E = EXPOSURE
E = EXPOSURE
Examination should be thorough whilst maintaining privacy and dignity(Based on UK Resuscitation Council 2010)despite the need for emergency treatment and care, basic needs such as information and support are not forgotten. As with all resuscitation situations a member of the multidisciplinary team should take responsibility for the provision of information and reassurance; it is a frighten- ing situation for the woman and any family members present at the time and they will all need compassionate support throughout. It is also helpful for women to have clear explanations when they are sufficiently recovered to be able to discuss what happened to them. Record keeping is also a vital function and a member of the inter-professional team should be allocated to ensure that all actions and treatments are carefully and accurately recorded.
Maternal resuscitation
The incidence of cardiopulmonary arrest is rare in pregnancy and childbirth and is most stronglyassociated with the birth itself. Although it is a rare occurrence, Billington and Stevenson (2007) suggest that the incidence is approximately 1:30,000; the outcomes are poor, but regular updat- ing of knowledge and skills by staff is the best method of maximising the chance of survival (Boyle and Yerby 2011; Centre for Maternal and Child Enquiries (CMACE) 2011). It is also vital to ensure that equipment is checked and maintained regularly and that all staff is fully aware of emergency telephone numbers.The Confidential Enquiry into Maternal Deaths (CMACE 2011) identifies both direct and indi- rect causes of death during pregnancy, childbirth and the postnatal period and those most likely to result in a need for resuscitation are listed below.
Maternal resuscitation
The incidence of cardiopulmonary arrest is rare in pregnancy and childbirth and is most stronglyassociated with the birth itself. Although it is a rare occurrence, Billington and Stevenson (2007) suggest that the incidence is approximately 1:30,000; the outcomes are poor, but regular updat- ing of knowledge and skills by staff is the best method of maximising the chance of survival (Boyle and Yerby 2011; Centre for Maternal and Child Enquiries (CMACE) 2011). It is also vital to ensure that equipment is checked and maintained regularly and that all staff is fully aware of emergency telephone numbers.The Confidential Enquiry into Maternal Deaths (CMACE 2011) identifies both direct and indi- rect causes of death during pregnancy, childbirth and the postnatal period and those most likely to result in a need for resuscitation are listed below.
Other books
I.D. by Vicki Grant
The Adulterer's Unofficial Guide to Family Vacations, A Novel by Langtry, Leslie
The St. Tropez Lonely Hearts Club by Joan Collins
Slam by Nick Hornby
A Perfect Love by Becca Lee, Hot Tree Editing, Lm Creations
The Winnowing Season by Cindy Woodsmall
Christie Ridgway by Must Love Mistletoe
The Art of Falling by Kathryn Craft
The Dead Ground by Claire Mcgowan
Gilded Lily by Delphine Dryden