Fundamentals of Midwifery: A Textbook for Students (83 page)
Read Fundamentals of Midwifery: A Textbook for Students Online
Authors: Louise Lewis

BOOK: Fundamentals of Midwifery: A Textbook for Students
9.83Mb size Format: txt, pdf, ePub
explain the links between physiological processes in the early days of life and the wellbeing of the newborn baby
discuss the care of the newborn immediately after birth
discuss the care of the newborn in the postnatal period
monitor the wellbeing of the newborn and recognise deviations from the normal
provide evidence-based information for parents.
Introduction
Although the majority of the care provided to newborn babies is given by their mothers, themidwife still plays an important role in ensuring that the health and wellbeing of the baby is monitored and that mothers and their families are provided with evidence-based information to support them in caring for their new baby. Some babies, although generally healthy, will need extra care and interventions from midwives such as basic resuscitation and screening tests. This chapter will provide an overview of the key aspects of care of the newborn infant. It does not address the care of the preterm or sick neonate, but aims to address the needs of the healthy, term baby whilst providing some insight into recognition of deviations from the normal in the early neonatal period.
Transition to extra-uterine life
Care of the baby following birth and in the postnatal period should be underpinned by knowl-edge of the process of change associated with a transition from uterine to extra-uterine life. The majority of neonates progress through this complex process without any problems, but those
 Fundamentals of Midwifery: A Textbook for Students
Fundamentals of Midwifery: A Textbook for Students
, First Edition. Edited by Louise Lewis.© 2015 John Wiley & Sons, Ltd. Published 2015 by John Wiley & Sons, Ltd. Companion website: www.wileyfundamentalseries.com/midwiferywho do experience difficulties will require appropriate and prompt intervention to minimise the effects on their development. In some cases delay or difficulties associated with transition can be as a result of congenital abnormality such as cardiac anomalies, prematurity or as a result of maternal ill health during pregnancy. These issues are generally known about prior to labour and delivery and therefore the care needs of the infant can be planned for. However it is impor- tant that the transition to extra-uterine life is not taken for granted in the absence of known risk factors. Midwives need to be prepared for and skilled in providing newborn resuscitation and recognising deviation from normal progress during the postnatal period. Resuscitation equipment should always be checked regularly to ensure that it is ready for use at all times.
Fetal circulation
Fetal circulation differs from adult circulation in order to facilitate oxygenation and nutrition viathe placenta. This is achieved by means of three temporary structures which are:
Introduction
Although the majority of the care provided to newborn babies is given by their mothers, themidwife still plays an important role in ensuring that the health and wellbeing of the baby is monitored and that mothers and their families are provided with evidence-based information to support them in caring for their new baby. Some babies, although generally healthy, will need extra care and interventions from midwives such as basic resuscitation and screening tests. This chapter will provide an overview of the key aspects of care of the newborn infant. It does not address the care of the preterm or sick neonate, but aims to address the needs of the healthy, term baby whilst providing some insight into recognition of deviations from the normal in the early neonatal period.
Transition to extra-uterine life
Care of the baby following birth and in the postnatal period should be underpinned by knowl-edge of the process of change associated with a transition from uterine to extra-uterine life. The majority of neonates progress through this complex process without any problems, but those
 Fundamentals of Midwifery: A Textbook for Students
Fundamentals of Midwifery: A Textbook for Students, First Edition. Edited by Louise Lewis.© 2015 John Wiley & Sons, Ltd. Published 2015 by John Wiley & Sons, Ltd. Companion website: www.wileyfundamentalseries.com/midwiferywho do experience difficulties will require appropriate and prompt intervention to minimise the effects on their development. In some cases delay or difficulties associated with transition can be as a result of congenital abnormality such as cardiac anomalies, prematurity or as a result of maternal ill health during pregnancy. These issues are generally known about prior to labour and delivery and therefore the care needs of the infant can be planned for. However it is impor- tant that the transition to extra-uterine life is not taken for granted in the absence of known risk factors. Midwives need to be prepared for and skilled in providing newborn resuscitation and recognising deviation from normal progress during the postnatal period. Resuscitation equipment should always be checked regularly to ensure that it is ready for use at all times.
Fetal circulation
Fetal circulation differs from adult circulation in order to facilitate oxygenation and nutrition viathe placenta. This is achieved by means of three temporary structures which are:
The ductus venosus
which shunts oxygenated blood from the placenta away from the liver.
which shunts oxygenated blood from the placenta away from the liver.
The foramen ovale
which allows oxygenated blood entering the right atria from the pla-centa via the inferior vena cava to shunt across to the left atria and therefore to enter the systemic circulation and bypass the pulmonary circulation.
which allows oxygenated blood entering the right atria from the pla-centa via the inferior vena cava to shunt across to the left atria and therefore to enter the systemic circulation and bypass the pulmonary circulation.
The ductus arteriosus
which shunts blood from the pulmonary artery into the aorta; thisalso facilitates oxygenated blood exiting from the right side of the heart entering the systemic circulation and therefore mostly bypassing the lungs.These fetal structures are essential for ensuring that oxygenated blood is circulated to where it is needed for growth and development. See Figure 9.1 for an illustration of the fetal circulation.
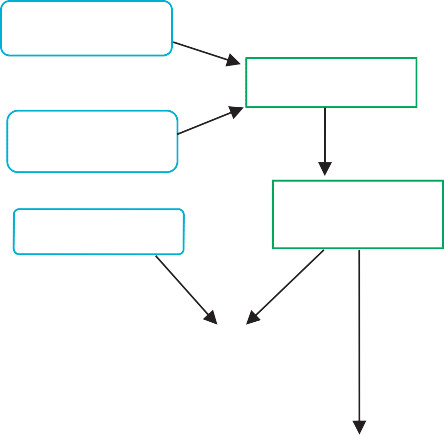
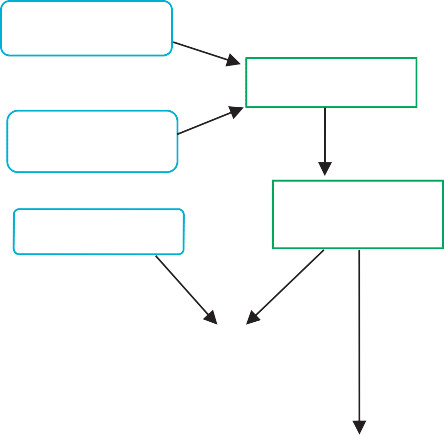
Transition
The transition from fetal circulation to extra-uterine circulation takes approximately a week to 10 days following birth. During labour the contractions and compression of the umbilical cord cause a rise in carbon dioxide and a fall in oxygen levels in the fetal blood; this situation is further exacerbated by clamping and cutting the cord at birth. As a result of this the respiratory centre is stimulated and this along with compression and release of the chest wall during birth stimu- late the infant to take its first breath. The lungs expand with the first breaths and there is an associated fall in pulmonary vascular resistance. The decrease in pressure in the right atrium results in constriction and then closure of the ductus venosus. Cutting the umbilical cord causes a rise in systemic blood pressure. The increased flow of blood to the lungs and back to the left atria causes a change of pressure within the heart which causes the ‘trapdoor’ of the foramen ovale to close; this occurs within 24–48 hours after birth. In some infants this closure does not occur and this may cause problems with disrupted flow of blood in early childhood, or may remain undetected until adulthood. Changes in flow and pressure also cause minimal flow in the ductus arteriosus. The oxygen saturations rise to normal limits as the extra-uterine circula- tion takes over and this causes a fall in the production of prostaglandin E
2
which results in closure of the ductus during the first week or 10 days of life (see Figure 9.2, which illustrates this process). The ductus is usually obliterated by three weeks of age.
Apgar scoring
The Apgar score was devised by the anaesthetist Virginia Apgar in 1952 and was introduced asa grading system of the newborn to allow a comparison and discussion of the results of obstetric
 189Ductus arteriosus Superior vena cava
189Ductus arteriosus Superior vena cava
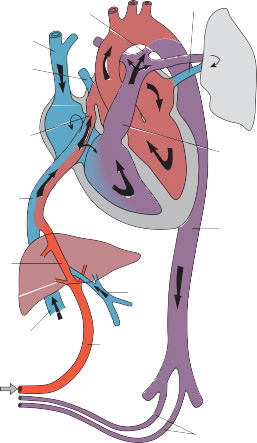 Pulmonary veinPulmonary vein
Pulmonary veinPulmonary vein
 190Oval foramenPulmonary arteryInferior vena cavaDescending aortaDuctus venosusPortal veinInferior vena cavaUmbilical veinUmbilical arteries
190Oval foramenPulmonary arteryInferior vena cavaDescending aortaDuctus venosusPortal veinInferior vena cavaUmbilical veinUmbilical arteries
Figure 9.1
Fetal circulation. Source: Sinha et al. 2012, Figure 1.2, p. 3. Reproduced with permission of John Wiley & Sons.practice, maternal analgesia and effects of resuscitation (Apgar 1953). It utilises a simple scoring system of five features of the infant at birth, which are assessed and recorded at one minute of age and then at five-minute intervals for the duration of any resuscitative measures. These features are heart rate, respiratory effort, response to stimulus, muscle tone and colour, each of which is scored out of two to give an overall score out of ten (Table 9.1).The National Institute for Health and Care Excellence guideline for intrapartum care (NICE 2007) instructs that the Apgar score at one and five minutes should be recorded routinely, although its value has been questioned and debated (Marlow 1992) because the assessment is made by those involved in the resuscitation and is rarely used contemporaneously to direct how the resuscitation should proceed, but retrospectively using recollection of those present. Other reports suggest that the person conducting the birth should not be the one to evaluate the score as they are often performing other duties and may introduce bias (Montgomery 2000), but in some maternity units this may be the only professional present at the birth. It should not be considered a measure of outcome or prognosis; the score does provide a useful indicator of condition at birth and highlights those babies who need closer monitoring in the early neonatal period. A score of under seven is considered low and under four very low with the lower scores
 High CO
High CO
2
and low O
2
during labour and birth stimulate respiratory centre in the brainFirst breathes inflate the lungs and reduce pulmonary vascular resistanceChest compression and release at delivery stimulates inspirationand clears alveolar fluid.Clamping and cutting cord raises systemic blood pressureReduced pulmonary resistance and decreased pressure in right atrium cause closure of ductus venosus and increased blood flow to lungs.
 191Increased pulmonary return and raised blood pressure increases pressure in the left atrium and foramen ovale ‘trapdoor’ closes during first few days of life.Increased O
191Increased pulmonary return and raised blood pressure increases pressure in the left atrium and foramen ovale ‘trapdoor’ closes during first few days of life.Increased O
2
saturation reduces prostaglandin E
2
production and therefore closes ductus arteriosus.
Figure 9.2
Transition to extra-uterine life.
Table 9.1
Agpar scoring
0
1
2
Heart rate
Absent
<100 bpm
>100 bpm
Respiratory effort
Absent
Slow, irregular
Regular, crying
Tone
Flaccid
Some flexion
Active
Response to stimulus
None
Grimace
Cough, cry
Colour
Blue/pale
Body pink, limbs blue
Pink
192having more significance for neurological sequalae when recorded at five and ten minutes of age (Thorngren-Jerneck and Herbst 2001).In practice, the most common problem is the tendency to evaluate the initial score sooner than one minute as in reality this is a longer period than it seems. The evaluation at five minutes of age may coincide with the timing of the delivery of the placenta and again is often calculated retrospectively, but if no resuscitative measures have been required by this time then the infant has not given any cause for concern and will not have a low Apgar score.
Basic resuscitation of the newborn
 It is estimated that only 10% of newborns will require some form of resuscitation (Fernandes2012), but it is not always possible to predict which babies these will be prior to birth. Midwives Rules and Standards (Nursing and Midwifery Council (NMC) 2012) state that a practising midwife is responsible for care of both woman and child during childbirth therefore every midwife has a responsibility to keep up to date with the principles of basic resuscitation.If a baby is born and does not spontaneously establish respiration within one minute, further assessment is required. During this first minute the actions of drying the baby and changing to fresh warm towels gives the opportunity to assess colour, tone, heart rate and respiratory effort. The heart rate is the most important of these signs and if this remains above 100 bpm in a baby with reasonable tone, some further time may be allowed for the baby to breathe spontaneously. Most will achieve this within 90 seconds.If a baby at birth is pale, floppy and bradycardic, then it is likely to need resuscitation, so help should be called for if not already in attendance. Even though this would seem to call for more immediate action, it is important to remember that the initial action of drying and changing to dry warm towels is still vital as hypothermia has a significant effect on the success of resuscita- tive measures. The only caveat to this is in the event of prematurity where it may be the policy to wrap the infant in an occlusive material such as plastic rather than drying the skin, or if there has been meconium present in the liquor as this is the one situation where suction is indicated and stimulus is initially kept to a minimum.For a baby with no obvious risk factors prior to birth, who does not commence spontaneous respiration, there are a few basic measures to undertake, the first of which is correct positioning. A newborn skull has a large occiput due to the moulding of the birth process and this has the effect of pushing the head forward when laid flat, thus causing the chin to drop and the airway to become occluded. Placing the head in the neutral position, with the nose pointing directly at the ceiling will correct this, open the airway and may allow spontaneous respiration to occur. If this measure is not enough, the airway may still be partially occluded by the back of the tongue. Poor muscle tone that can be seen in the limbs is likely to be affecting internal structures equally so it is necessary to perform a chin lift by placing a finger under the bony tip of chin (making sure not to press on the soft tissues) or a jaw thrust manoeuvre to pull the bottom jaw forward and move the tongue. This is achieved by applying gentle pressure each side behind the angle of the lower mandible, just below the ears, in a forward motion. This action can be performed with the fingers whilst the thumbs are placed on the cheek bones.A baby that is still not breathing despite an open airway will need to have their lungs inflated for them. This is performed using a face mask and positive pressure, in the hospital setting provided by a resuscitaire; in the community setting this may be by bag and face mask or port- able ventilation equipment. The recommendations are that this is initially performed using air, with the addition of oxygen only if required (World Health Organization (WHO) 2012; Resuscita- tion Council (UK) 2010).As it is not possible to predict which babies are going to need assistance to establish respira- tion, it is important that the equipment has been checked prior to birth and the pressures set appropriately. The pressure required for initial inflation of the newborn lungs of a term baby is 30 cm/H
It is estimated that only 10% of newborns will require some form of resuscitation (Fernandes2012), but it is not always possible to predict which babies these will be prior to birth. Midwives Rules and Standards (Nursing and Midwifery Council (NMC) 2012) state that a practising midwife is responsible for care of both woman and child during childbirth therefore every midwife has a responsibility to keep up to date with the principles of basic resuscitation.If a baby is born and does not spontaneously establish respiration within one minute, further assessment is required. During this first minute the actions of drying the baby and changing to fresh warm towels gives the opportunity to assess colour, tone, heart rate and respiratory effort. The heart rate is the most important of these signs and if this remains above 100 bpm in a baby with reasonable tone, some further time may be allowed for the baby to breathe spontaneously. Most will achieve this within 90 seconds.If a baby at birth is pale, floppy and bradycardic, then it is likely to need resuscitation, so help should be called for if not already in attendance. Even though this would seem to call for more immediate action, it is important to remember that the initial action of drying and changing to dry warm towels is still vital as hypothermia has a significant effect on the success of resuscita- tive measures. The only caveat to this is in the event of prematurity where it may be the policy to wrap the infant in an occlusive material such as plastic rather than drying the skin, or if there has been meconium present in the liquor as this is the one situation where suction is indicated and stimulus is initially kept to a minimum.For a baby with no obvious risk factors prior to birth, who does not commence spontaneous respiration, there are a few basic measures to undertake, the first of which is correct positioning. A newborn skull has a large occiput due to the moulding of the birth process and this has the effect of pushing the head forward when laid flat, thus causing the chin to drop and the airway to become occluded. Placing the head in the neutral position, with the nose pointing directly at the ceiling will correct this, open the airway and may allow spontaneous respiration to occur. If this measure is not enough, the airway may still be partially occluded by the back of the tongue. Poor muscle tone that can be seen in the limbs is likely to be affecting internal structures equally so it is necessary to perform a chin lift by placing a finger under the bony tip of chin (making sure not to press on the soft tissues) or a jaw thrust manoeuvre to pull the bottom jaw forward and move the tongue. This is achieved by applying gentle pressure each side behind the angle of the lower mandible, just below the ears, in a forward motion. This action can be performed with the fingers whilst the thumbs are placed on the cheek bones.A baby that is still not breathing despite an open airway will need to have their lungs inflated for them. This is performed using a face mask and positive pressure, in the hospital setting provided by a resuscitaire; in the community setting this may be by bag and face mask or port- able ventilation equipment. The recommendations are that this is initially performed using air, with the addition of oxygen only if required (World Health Organization (WHO) 2012; Resuscita- tion Council (UK) 2010).As it is not possible to predict which babies are going to need assistance to establish respira- tion, it is important that the equipment has been checked prior to birth and the pressures set appropriately. The pressure required for initial inflation of the newborn lungs of a term baby is 30 cm/H
which shunts blood from the pulmonary artery into the aorta; thisalso facilitates oxygenated blood exiting from the right side of the heart entering the systemic circulation and therefore mostly bypassing the lungs.These fetal structures are essential for ensuring that oxygenated blood is circulated to where it is needed for growth and development. See Figure 9.1 for an illustration of the fetal circulation.
Transition
The transition from fetal circulation to extra-uterine circulation takes approximately a week to 10 days following birth. During labour the contractions and compression of the umbilical cord cause a rise in carbon dioxide and a fall in oxygen levels in the fetal blood; this situation is further exacerbated by clamping and cutting the cord at birth. As a result of this the respiratory centre is stimulated and this along with compression and release of the chest wall during birth stimu- late the infant to take its first breath. The lungs expand with the first breaths and there is an associated fall in pulmonary vascular resistance. The decrease in pressure in the right atrium results in constriction and then closure of the ductus venosus. Cutting the umbilical cord causes a rise in systemic blood pressure. The increased flow of blood to the lungs and back to the left atria causes a change of pressure within the heart which causes the ‘trapdoor’ of the foramen ovale to close; this occurs within 24–48 hours after birth. In some infants this closure does not occur and this may cause problems with disrupted flow of blood in early childhood, or may remain undetected until adulthood. Changes in flow and pressure also cause minimal flow in the ductus arteriosus. The oxygen saturations rise to normal limits as the extra-uterine circula- tion takes over and this causes a fall in the production of prostaglandin E
2
which results in closure of the ductus during the first week or 10 days of life (see Figure 9.2, which illustrates this process). The ductus is usually obliterated by three weeks of age.
Apgar scoring
The Apgar score was devised by the anaesthetist Virginia Apgar in 1952 and was introduced asa grading system of the newborn to allow a comparison and discussion of the results of obstetric
 189Ductus arteriosus Superior vena cava
189Ductus arteriosus Superior vena cava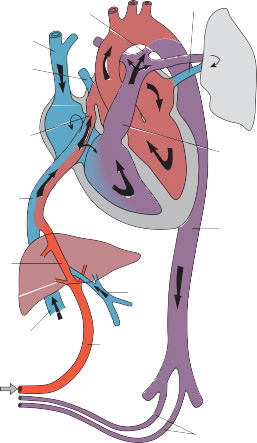 Pulmonary veinPulmonary vein
Pulmonary veinPulmonary vein 190Oval foramenPulmonary arteryInferior vena cavaDescending aortaDuctus venosusPortal veinInferior vena cavaUmbilical veinUmbilical arteries
190Oval foramenPulmonary arteryInferior vena cavaDescending aortaDuctus venosusPortal veinInferior vena cavaUmbilical veinUmbilical arteriesFigure 9.1
Fetal circulation. Source: Sinha et al. 2012, Figure 1.2, p. 3. Reproduced with permission of John Wiley & Sons.practice, maternal analgesia and effects of resuscitation (Apgar 1953). It utilises a simple scoring system of five features of the infant at birth, which are assessed and recorded at one minute of age and then at five-minute intervals for the duration of any resuscitative measures. These features are heart rate, respiratory effort, response to stimulus, muscle tone and colour, each of which is scored out of two to give an overall score out of ten (Table 9.1).The National Institute for Health and Care Excellence guideline for intrapartum care (NICE 2007) instructs that the Apgar score at one and five minutes should be recorded routinely, although its value has been questioned and debated (Marlow 1992) because the assessment is made by those involved in the resuscitation and is rarely used contemporaneously to direct how the resuscitation should proceed, but retrospectively using recollection of those present. Other reports suggest that the person conducting the birth should not be the one to evaluate the score as they are often performing other duties and may introduce bias (Montgomery 2000), but in some maternity units this may be the only professional present at the birth. It should not be considered a measure of outcome or prognosis; the score does provide a useful indicator of condition at birth and highlights those babies who need closer monitoring in the early neonatal period. A score of under seven is considered low and under four very low with the lower scores
 High CO
High CO2
and low O
2
during labour and birth stimulate respiratory centre in the brainFirst breathes inflate the lungs and reduce pulmonary vascular resistanceChest compression and release at delivery stimulates inspirationand clears alveolar fluid.Clamping and cutting cord raises systemic blood pressureReduced pulmonary resistance and decreased pressure in right atrium cause closure of ductus venosus and increased blood flow to lungs.
 191Increased pulmonary return and raised blood pressure increases pressure in the left atrium and foramen ovale ‘trapdoor’ closes during first few days of life.Increased O
191Increased pulmonary return and raised blood pressure increases pressure in the left atrium and foramen ovale ‘trapdoor’ closes during first few days of life.Increased O2
saturation reduces prostaglandin E
2
production and therefore closes ductus arteriosus.
Figure 9.2
Transition to extra-uterine life.
Table 9.1
Agpar scoring
0
1
2
Heart rate
Absent
<100 bpm
>100 bpm
Respiratory effort
Absent
Slow, irregular
Regular, crying
Tone
Flaccid
Some flexion
Active
Response to stimulus
None
Grimace
Cough, cry
Colour
Blue/pale
Body pink, limbs blue
Pink
192having more significance for neurological sequalae when recorded at five and ten minutes of age (Thorngren-Jerneck and Herbst 2001).In practice, the most common problem is the tendency to evaluate the initial score sooner than one minute as in reality this is a longer period than it seems. The evaluation at five minutes of age may coincide with the timing of the delivery of the placenta and again is often calculated retrospectively, but if no resuscitative measures have been required by this time then the infant has not given any cause for concern and will not have a low Apgar score.
Basic resuscitation of the newborn
 It is estimated that only 10% of newborns will require some form of resuscitation (Fernandes2012), but it is not always possible to predict which babies these will be prior to birth. Midwives Rules and Standards (Nursing and Midwifery Council (NMC) 2012) state that a practising midwife is responsible for care of both woman and child during childbirth therefore every midwife has a responsibility to keep up to date with the principles of basic resuscitation.If a baby is born and does not spontaneously establish respiration within one minute, further assessment is required. During this first minute the actions of drying the baby and changing to fresh warm towels gives the opportunity to assess colour, tone, heart rate and respiratory effort. The heart rate is the most important of these signs and if this remains above 100 bpm in a baby with reasonable tone, some further time may be allowed for the baby to breathe spontaneously. Most will achieve this within 90 seconds.If a baby at birth is pale, floppy and bradycardic, then it is likely to need resuscitation, so help should be called for if not already in attendance. Even though this would seem to call for more immediate action, it is important to remember that the initial action of drying and changing to dry warm towels is still vital as hypothermia has a significant effect on the success of resuscita- tive measures. The only caveat to this is in the event of prematurity where it may be the policy to wrap the infant in an occlusive material such as plastic rather than drying the skin, or if there has been meconium present in the liquor as this is the one situation where suction is indicated and stimulus is initially kept to a minimum.For a baby with no obvious risk factors prior to birth, who does not commence spontaneous respiration, there are a few basic measures to undertake, the first of which is correct positioning. A newborn skull has a large occiput due to the moulding of the birth process and this has the effect of pushing the head forward when laid flat, thus causing the chin to drop and the airway to become occluded. Placing the head in the neutral position, with the nose pointing directly at the ceiling will correct this, open the airway and may allow spontaneous respiration to occur. If this measure is not enough, the airway may still be partially occluded by the back of the tongue. Poor muscle tone that can be seen in the limbs is likely to be affecting internal structures equally so it is necessary to perform a chin lift by placing a finger under the bony tip of chin (making sure not to press on the soft tissues) or a jaw thrust manoeuvre to pull the bottom jaw forward and move the tongue. This is achieved by applying gentle pressure each side behind the angle of the lower mandible, just below the ears, in a forward motion. This action can be performed with the fingers whilst the thumbs are placed on the cheek bones.A baby that is still not breathing despite an open airway will need to have their lungs inflated for them. This is performed using a face mask and positive pressure, in the hospital setting provided by a resuscitaire; in the community setting this may be by bag and face mask or port- able ventilation equipment. The recommendations are that this is initially performed using air, with the addition of oxygen only if required (World Health Organization (WHO) 2012; Resuscita- tion Council (UK) 2010).As it is not possible to predict which babies are going to need assistance to establish respira- tion, it is important that the equipment has been checked prior to birth and the pressures set appropriately. The pressure required for initial inflation of the newborn lungs of a term baby is 30 cm/H
It is estimated that only 10% of newborns will require some form of resuscitation (Fernandes2012), but it is not always possible to predict which babies these will be prior to birth. Midwives Rules and Standards (Nursing and Midwifery Council (NMC) 2012) state that a practising midwife is responsible for care of both woman and child during childbirth therefore every midwife has a responsibility to keep up to date with the principles of basic resuscitation.If a baby is born and does not spontaneously establish respiration within one minute, further assessment is required. During this first minute the actions of drying the baby and changing to fresh warm towels gives the opportunity to assess colour, tone, heart rate and respiratory effort. The heart rate is the most important of these signs and if this remains above 100 bpm in a baby with reasonable tone, some further time may be allowed for the baby to breathe spontaneously. Most will achieve this within 90 seconds.If a baby at birth is pale, floppy and bradycardic, then it is likely to need resuscitation, so help should be called for if not already in attendance. Even though this would seem to call for more immediate action, it is important to remember that the initial action of drying and changing to dry warm towels is still vital as hypothermia has a significant effect on the success of resuscita- tive measures. The only caveat to this is in the event of prematurity where it may be the policy to wrap the infant in an occlusive material such as plastic rather than drying the skin, or if there has been meconium present in the liquor as this is the one situation where suction is indicated and stimulus is initially kept to a minimum.For a baby with no obvious risk factors prior to birth, who does not commence spontaneous respiration, there are a few basic measures to undertake, the first of which is correct positioning. A newborn skull has a large occiput due to the moulding of the birth process and this has the effect of pushing the head forward when laid flat, thus causing the chin to drop and the airway to become occluded. Placing the head in the neutral position, with the nose pointing directly at the ceiling will correct this, open the airway and may allow spontaneous respiration to occur. If this measure is not enough, the airway may still be partially occluded by the back of the tongue. Poor muscle tone that can be seen in the limbs is likely to be affecting internal structures equally so it is necessary to perform a chin lift by placing a finger under the bony tip of chin (making sure not to press on the soft tissues) or a jaw thrust manoeuvre to pull the bottom jaw forward and move the tongue. This is achieved by applying gentle pressure each side behind the angle of the lower mandible, just below the ears, in a forward motion. This action can be performed with the fingers whilst the thumbs are placed on the cheek bones.A baby that is still not breathing despite an open airway will need to have their lungs inflated for them. This is performed using a face mask and positive pressure, in the hospital setting provided by a resuscitaire; in the community setting this may be by bag and face mask or port- able ventilation equipment. The recommendations are that this is initially performed using air, with the addition of oxygen only if required (World Health Organization (WHO) 2012; Resuscita- tion Council (UK) 2010).As it is not possible to predict which babies are going to need assistance to establish respira- tion, it is important that the equipment has been checked prior to birth and the pressures set appropriately. The pressure required for initial inflation of the newborn lungs of a term baby is 30 cm/HOther books
Red Red Rose by Stephanie Hoffman McManus
The House of Grey- Volume 3 by Earl, Collin
Versions (The Blacklist Series Book 1) by Mitcham, Megan
Betrothed by Renee Rose
The Lost by Vicki Pettersson
Softly Grow the Poppies by Audrey Howard
Four Weeks by Melissa Ford
Styx by Bavo Dhooge
Night of the Jaguar by Michael Gruber
Loom and Doom by Carol Ann Martin