Resident Readiness General Surgery (30 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

Six days later, while on call for the general surgery service, you are asked to evaluate the same patient who has been recovering uneventfully until now. He complains of new mild pelvic discomfort, anorexia, and difficulty voiding. His bowel function has not yet returned. He has a low-grade fever, mild tachycardia, and moderate right lower quadrant tenderness to deep palpation. A CBC with differential reveals leukocytosis with neutrophil predominance. CT of his abdomen and pelvis with oral and intravenous contrast reveals a 6-cm rim-enhancing pelvic fluid collection surrounding the rectal stump (see
Figure 22-1
).
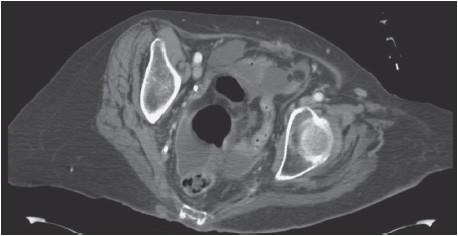
Figure 22-1.
Axial CT of a postoperative pelvic fluid collection.
1.
Does this patient have an abscess or does he have a phlegmon?
2.
Would this fluid collection be classified as primary, secondary, or tertiary?
3.
Why does this patient have an ileus?
4.
Is it reasonable to treat this patient with antibiotics alone?
5.
What class of microbes should you cover with antibiotics?
6.
Would you order this patient’s CT with oral, IV, or both types of contrast?
7.
Based on the available CT imaging, do you think your interventional radiology (IR) colleagues would agree to drain this abscess percutaneously?
INTRA-ABDOMINAL ABSCESS
Answers
1.
An intra-abdominal abscess (IAA) is a contained collection of infected fluid within the confines of the peritoneal cavity, with or without associated pockets of gas. A phlegmon, in contrast, is an inflammatory mass without identifiable fluid. The patient in the case vignette has IAA.
2.
There are several ways to classify IAA, although the etiologic classification is the most common:
•
Primary IAAs are monomicrobial infections that arise spontaneously without any identifiable breach of the gastrointestinal tract. Spontaneous bacterial peritonitis is an example of a primary IAA.
•
Secondary IAAs result from spontaneous, surgical, or iatrogenic violation of the gastrointestinal tract and account for the overwhelming majority of abscesses encountered by the surgeon. Diverticular abscesses are a common example of secondary IAA.
•
Tertiary IAAs are recurrent infections following treatment of primary or secondary abscesses. These recalcitrant IAAs typically contain antibiotic-resistant nosocomial infections.
Given the relative infrequency of primary and tertiary abscesses, this chapter will focus on secondary IAA, and more specifically on intraperitoneal secondary IAA, which is present in the patient in the case vignette.
3.
IAA may present with a wide range of clinical manifestations. Classic findings for spontaneous IAA include fever, lethargy, leukocytosis, and abdominal pain or fullness. Rarely, IAA may present with overt peritonitis or sepsis. The local inflammation can cause changes in bowel habits, including nausea, vomiting, diarrhea, or constipation. Similarly, a prolonged postoperative ileus can often be the initial manifestation of postoperative IAA, as is the case in this vignette. Subphrenic abscesses can cause hiccups and a sympathetic pleural effusion, while pelvic abscesses can cause tenesmus, lower back pain, and urinary retention. Physical exam may reveal focal tenderness or occasionally a palpable abdominal mass, while low pelvic abscesses may be palpated on digital rectal exam.
4.
Generally no. Systemic antibiotic therapy is thought to have poor penetration into an abscess cavity for several reasons. First, host neutrophils form an inflammatory rind of fibrin that encases and entraps the collection, walling the cavity off from host circulation and preventing penetration of circulating antibiotic. It also markedly reduces the oxygen available in the cavity, and as a consequence of these anaerobic conditions, the abscess cavity contents are usually acidic. This acid further reduces the efficacy of any antibiotic that does manage to penetrate the cavity.
For these reasons, classical surgical dogma states that antibiotics alone are not helpful and recommend source control via abscess drainage. Antibiotics should still be used, but only as adjunctive treatment for IAA in order to prevent extension of infection into the surrounding soft tissue. There are a few narrow circumstances, however, where it may be appropriate to violate the classical dogma and treat with antibiotics alone. For example, immunocompetent patients who only have small abscesses and do not have any other concerning signs (eg, peritonitis, sepsis) may not require drainage for full recovery. It bears emphasizing, however, that any patient with sepsis, peritonitis, or evidence of end-organ dysfunction requires emergent (likely surgical) drainage—in those cases, antibiotic therapy alone is typically not helpful.
5.
Virtually all secondary IAAs contain gut flora. Common aerobes include
Escherichia coli
,
Enterococcus
, and
Klebsiella
species while common anaerobes include
Bacteroides fragilis
and
Peptostreptococcus
species. Suitable first-line antimicrobials include piperacillin–tazobactam, ticarcillin–clavulanate, ertapenem, or tigecycline as single-agent therapy, or combinations of metronidazole with cefazolin, cefuroxime, levofloxacin, or ciprofloxacin.
6.
Both types of contrast should be used. Contemporary CT imaging can accurately diagnose IAA with a sensitivity and specificity that exceeds 90%. In the stable patient without indication for immediate surgical exploration, cross-sectional imaging presents important data to the surgeon regarding underlying abscess etiology and may provide nonoperative treatment alternatives that may obviate or temporize surgery until conditions are ideal. In special circumstances, ultrasound may play an ancillary role in diagnosing IAA with slightly lower accuracy rates compared with CT or MRI.
IAAs are defined on CT as a fluid collection with or without associated pockets of gas. An abscess is in contradistinction to a phlegmon, which is an inflammatory mass without identifiable fluid. Enteral contrast (either oral or rectal) can be a helpful adjunct that distinguishes loops of bowel from the abscess cavity and may provocatively assess anastomoses for leaks or fistulae. Intravenous contrast provides a pathognomonic “rim enhancement” that is seen along the outer rind of the abscess cavity. Abscess architecture can be classified as simple or loculated, referring to the degree of internal pockets or presence of septae. The location of the abscess, both absolute and relative to other organs, can be assessed and may diagnose the pathology responsible for the abscess (see
Figure 22-2
).
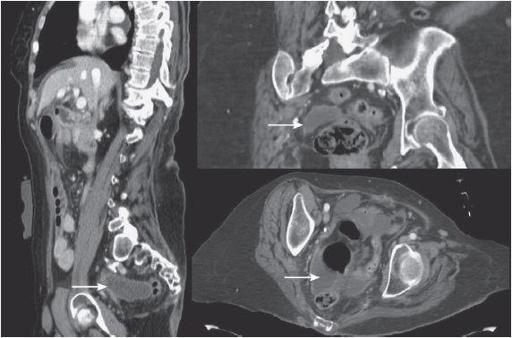
Figure 22-2.
Axial, coronal, and sagittal CT reconstructions of a postoperative pelvic abscess.
7.
The development of percutaneous image-guided drainage techniques in the early 1980s has markedly impacted the management of IAA. Prior to the advent of cross-sectional imaging, the diagnosis and management of IAA often required surgical reexploration that conveyed mortality rates as high as 40%.
IAA with favorable characteristics can often be managed with image-guided drain placement. Ideally, the target fluid collection must be well circumscribed and have radiographic characteristics of an abscess, rather than free ascites. There must be a radiographic window that permits a safe percutaneous trajectory for real-time image-guided needle passage without causing injury to other structures. Abscesses typically must be larger than 4 cm for consideration of drain placement, although smaller abscesses can be aspirated without placement of a drain or treated with antibiotics alone. Solitary, noncomplex, nonloculated abscesses are ideal candidates for successful image-guided drainage procedures with success rates of approximately 80%.
TIPS TO REMEMBER
IAAs with sepsis, peritonitis, or failing nonoperative management typically require prompt resuscitation and surgical exploration.
Image-guided drain placement is suitable for stable patients with confirmed abscess >4 cm. Smaller fluid collections can be aspirated under image guidance or treated with antibiotics alone.
Antibiotic therapy alone is only helpful for small abscesses or phlegmons. Larger abscesses require drainage via percutaneous or surgical approaches with antibiotics relegated to an adjunctive role.
Some abscess locations will not permit a safe radiographic window or trajectory for image-guided drainage and may require surgical drainage.