Resident Readiness General Surgery (33 page)
Read Resident Readiness General Surgery Online
Authors: Debra Klamen,Brian George,Alden Harken,Debra Darosa
Tags: #Medical, #Surgery, #General, #Test Preparation & Review

Shamim H. Nejad, MD and Justin B. Smith, MD
Mr. Thompkins is an otherwise healthy 72-year-old man who was admitted after experiencing 15% total body surface area burns to his trunk, arms, neck, and face. He is now 2 days s/p excision and grafting of his injuries. His postoperative course was unremarkable until last evening when he became acutely confused. He stated that he was at the library and he was observed to be having conversations with people who were not there. The patient also began to pull at his lines and attempted to get out of bed. He required frequent redirection and reorienting by his nurse, which prompted a call to the night float resident. The nurse was particularly concerned that he may be in alcohol withdrawal as it was reported in his admission note that he consumed ethanol in “social situations.”
The night float resident initially gave the patient lorazepam 2 mg IV to sedate him. He was then placed on lorazepam 1 mg IV every 4 hours standing, along with PRN lorazepam ordered “per signs of alcohol withdrawal.” Despite these interventions the patient’s mental status continued to worsen, and on rounds the following morning your team discovers that he now requires oxygen supplementation. You review the rest of his medications and note that the patient is also on a hydromorphone PCA, which the nurse tells you she has been activating “to keep him comfortable” as the patient is too confused to use the PCA himself.
On physical examination, his vitals are T: 99.9, HR: 115, BP: 150/90, R: 16, and O
2
: 97% on 3 L of oxygen per nasal cannula. The patient is lying in bed with his eyes closed, although he can be aroused with loud verbal stimuli. He is oriented only to self and falls asleep repeatedly during the examination. When he is awake, he has difficulty maintaining focus and attention. Pupils are equal and reactive, and his cranial nerve examination is intact. Upper extremities are without cogwheeling, rigidity, or tremor. The patient displays a palmomental reflex bilaterally; however, no glabellar, snout, or plantar reflexes are noted. In addition, there are intermittent myoclonic jerks of the upper extremities and trunk.
Laboratory results are notable only for a WBC of 16,700 and a sodium of 129. A review of admission labs includes a normal MCV of 95, an ALT of 22, an AST of 28, and normal coagulation studies. A blood alcohol level along with a urine toxicology screen at the time of admission was negative.
1.
Based on the details given, does this patient meet the diagnostic criteria of delirium?
2.
Is delirium life-threatening?
3.
You’ve excluded any serious medical condition as the cause of his altered mental status (AMS). What else could be causing these changes?
4.
What is the first-line pharmaceutical agent for treatment of severe agitation?
5.
What are the most common risks associated with this agent?
ALTERED MENTAL STATUS
Answers
1.
In assessing mental status changes in the hospitalized patient it is important to distinguish delirium from other underlying psychiatric disorders. Delirium, as opposed to most other psychiatric disturbances, has an acute onset within hours to days, is caused by a medical condition, and is reversible. The cardinal sign of delirium is an altered level of consciousness accompanied by cognitive deficits that cannot be accounted for by a past or evolving dementia.
In the case example, this patient’s mental status changed acutely in the hours and days after surgery. The patient clearly demonstrated a continued disturbance of consciousness by falling asleep during the examination. In addition, he was disoriented and had difficulty maintaining focus and attention, all core features of delirium. He demonstrated cognitive deficits as noted by disorientation (thinking he was in the library, pulling out lines, requiring frequent redirection) and perceptual disturbances (having conversations with people who were not there).
2.
Delirium is a medical emergency and the underlying cause must be identified and treated. While the delirium itself is not usually life-threatening, it can be the first sign of a more serious condition such as hypotension, hypoxia, anemia/bleeding, or infection. As such, you should respond immediately whenever you are paged about a patient with AMS.
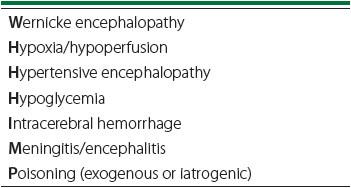
As you are evaluating the patient you should remember that there are seven states, designated by the mnemonic WHHHIMP (
Table 24-1
) that require immediate intervention to avoid death or permanent CNS damage.
Table 24-1.
High-risk Causes of AMS
Simply evaluating the time of onset and course of the patient’s symptoms can often lead to a preliminary diagnosis. But the diagnosis is not always so
simple—delirium can present in many different ways and psychiatrists refer to it as “the great imitator.” After obtaining a history you should examine the vital signs closely. The most worrisome finding is any evidence that suggests the delirium is the result of end-organ hypoperfusion, that is, shock. You should also note the presence or absence of fever (suggesting infection) or hypoxia (which can cause delirium directly). After reviewing the vital signs, the clinical evaluation should proceed with a complete neurological examination. In assessing the patient’s mental status you should evaluate the patient for paranoia or perceptual disturbances (either of which can cause patients to be quite agitated or even aggressive). Perceptual disturbances (most often visual hallucinations) are particularly notable as they are remarkably rare in primary psychiatric disturbances. While some patients are agitated, others may have a hypoactive delirium that goes unnoticed by staff because they are quietly confused. Physical examination should also include assessment for the presence of multifocal myoclonus, along with frontal release signs (palmomental, glabellar, and plantar reflexes). Positive findings are often associated with generalized encephalopathy (ie, frontal network syndrome caused by metabolic derangements, infection, or medications—opiates and benzodiazepines) and do not necessarily mean that there is an acute bleed or lesion. If there are any focal neurological deficits or you have any doubt as to the underlying etiology, then neurological or psychiatric consultation should be obtained.
In this patient, his level of consciousness was depressed and he required supplemental oxygen. These could be due to the medications he was being given (opiates and benzodiazepines) or could be the result of a pulmonary infection (note that his WBC is elevated). He also had both myoclonus and frontal release signs that suggest a nonfocal etiology such as medications, infection, or a metabolic cause. Looking at his labs, not only does he have the aforementioned leukocytosis but he also has a hyponatremia, one example of many possible metabolic causes of delirium.
The nurse was specifically concerned about alcohol withdrawal, an understandable concern given the timing of the AMS (alcohol withdrawal usually manifests 2-3 days after the last drink). However, prior to initiating
treatment
for alcohol withdrawal delirium it is mandatory to collect collateral history with regard to the patient’s alcohol use, particularly given the fact that this patient’s liver function tests, coagulation studies, and MCV were normal and the patient didn’t exhibit any symptoms of tremor or diaphoresis. In short, alcohol withdrawal delirium is a diagnosis of exclusion and should be based on clinical findings, laboratory findings, and, if possible, collateral history.
3.
If no medical cause can be identified (ie, you do not find evidence of one of the seven “high-risk” diagnoses, of infection, or of metabolic derangements), then the next step in management often involves simplifying the patient’s medication list. Pharmaceutical agents are among the most common iatrogenic causes of AMS, and reducing or eliminating offending agents is often very effective.
Many classes of medications can contribute to delirium. Classic examples include anticholinergic medications such as diphenhydramine (Benadryl) or promethazine (Phenergan). Narcotics (such as hydromorphone) are also a common culprit for AMS. While the use of narcotics in surgical patients is often mandatory to obtain adequate analgesia, care should be taken to ensure that the patient receives the lowest effective dosage of medication to achieve pain control. Lastly, benzodiazepines (such as lorazepam) can also precipitate or contribute to delirium.
As an adjunct to simplifying the medication list, environmental interventions can also be helpful. You should ensure that the patient has his or her hearing/visual aids, instruct the nurses to provide frequent reorientation, and optimize the sleep/wake cycle by minimizing unnecessary overnight disturbances.
In addition, certain surgical conditions associated with inflammatory states (long bone fractures, burn injuries, pancreatitis, etc) often lead to AMS. These conditions and their associated inflammatory response states may result in a significant proinflammatory cytokine-mediated process that leads to fenestrations in the blood–brain barrier with resulting CNS dysregulation in the limbic cortices, resulting in encephalopathy. In burn patients, AMS will often persist until all wounds are excised, grafted, and fully closed. Furthermore, whether related to traumatic surgical intervention, unplanned surgery, or an elective surgery,
any
operation results in an expected inflammation-mediated process that usually peaks on postoperative day 2, coinciding with the time of the highest incidence of postoperative delirium.
4.
The best option is to treat the delirium by treating the underlying medical cause. However, in some cases the underlying cause is not readily identifiable or rapidly reversible and pharmacologic treatment of the symptoms of delirium becomes necessary. This is particularly true for patients who are severely agitated and at risk of hurting themselves or others.
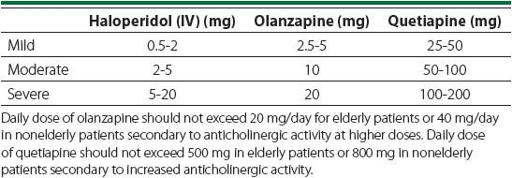
Dopamine antagonists are frequently used for the treatment of delirium. Haloperidol IV is the first-line agent for the treatment of agitated delirium, particularly in critical care settings given its relatively benign cardiopulmonary risk profile. It is also the primary agent for the treatment and management of severe agitation on the general care floor. When it is necessary to use an enteral formulation (due to preexisting hospital guidelines or attempting disposition to a rehabilitative facility), one may choose quetiapine (Seroquel) or olanzapine (Zyprexa). Quetiapine is generally preferred over olanzapine in patients with underlying neurodegenerative disorders due to its decreased affinity for dopa-mine blockage and less extrapyramidal symptom (EPS)–related side effects (see below). See
Table 24-2
for dosing strategies for these medications for the treatment of agitation.
Table 24-2.
Dosing Strategies for Agitation
Caution is warranted in the use of benzodiazepines such as lorazepam because they carry the risk of
worsening
an underlying delirium and increasing morbidity and mortality. They are also associated with respiratory depression
and should be avoided in patients with respiratory compromise. Benzodiazepines should therefore be reserved for those cases of severe agitation that are initially refractory to escalating doses of IV haloperidol. Even then they should only be used sparingly, while other interventions are aggressively attempted.
5.
While dopamine antagonists are relatively safe, it is important to understand their side effect profiles. The most significant risk associated with dopamine antagonists is their potential to cause EPS. This is particularly true of haloperidol. All dopamine antagonists also have QT prolonging effects and carry a theoretical risk of inducing
torsade de pointes
. To minimize the risk of QTc prolongation, potassium and magnesium repletion should be performed daily, avoidance and/or minimization of unnecessary QTc prolonging medications should be attempted, and a daily ECG should be performed to ensure it remains below 550 milliseconds. Sedation is also a side effect of the newer-generation dopamine antagonists, such as quetiapine and olanzapine, although this may actually be beneficial when treating a patient with delirium due to hyperarousal. Dopamine antagonists should be minimized in patients with Parkinson disease or other severe neurodegenerative disorders, and psychiatric consultation should be considered for assistance in management of these patients.