Secondary Schizophrenia (147 page)
Read Secondary Schizophrenia Online
Authors: Perminder S. Sachdev

but quite clear and occurred in overlapping sequence
with damage to the occipital lobe may
[62]
or may
A
→
B
→
C over a period of 10 to 12 days.
not
[19,
63]
show epileptiform discharges. Neverthe-When the primate visual area V1 is stained for
less, it has been repeatedly shown that isolated cortex
cytochrome oxidase, it is characterized by orderly rows
becomes epileptogenic
[64, 65].
of “blobs” with an arrangement both qualitatively and
A further elaboration of these ideas is to sug-
quantitatively similar to that of the “spots” shown in
gest that the more extensive the damage to the visual
Figure 30.2B.
Similarly, when visual area V2 is stained,
system, the higher in the visual hierarchy does the
it reveals an arrangement of stripes closely resem-
increased spontaneous activity extend and the more
bling in dimensions the brickwork shown in Figure
likely it is that the hallucinations will be complex.
30.2A. Cytochrome oxidase is an indicator of high
Leaves and branching structures might be located
371
metabolic rate and might be expected to signal the
higher than brick walls; people and buildings would be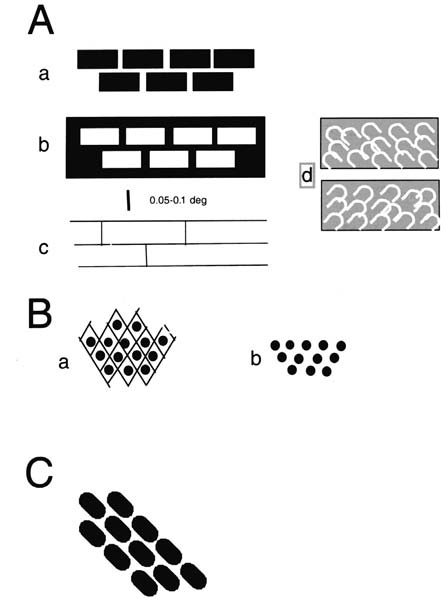
Related Concepts – Section 4
is this second model, which is appropriate for CBS,
and which I will explore in detail. Simply stated, the
deafferentation theory proposes that deafferentation
leads to hypersensitivity at the deafferented synapses
and this leads to increased spontaneous activity that is
the neural basis of the hallucinations. The fact that low
contrast sensitivity is a strong risk factor for CBS also
supports this theory
[72].
The deafferentation syndrome model has been
most successful when applied to the somatosensory
system, the best example being the “phantom limb”
phenomenon. When a patient loses a limb, the neurons
in the cerebral cortex that normally receive input from
the limb are still there and undamaged. Therefore, if
by any means they are excited, they will signal that the
limb is being touched or stimulated in some way. It
is irrelevant how the cortical neurons are excited; as
a result of deafferentation, they are likely to become
spontaneously active and this activity will create the
phantom. The theory was probably even more success-
ful in explaining the anomalies in pain sensation, for
example, how pain can be increased when the number
of pain receptors is decreased
[73].
Deafferentation in
the auditory system can lead to tinnitus and hallucinations
[74, 75, 76].
Occasionally, a combination of visual
Figure 30.2
Sketches of portions of hallucinations seen by the
and hearing loss leads to both visual and auditory hal-author over a period of 10–12 days following a macular hole in each
eye. The hallucinations appeared in the sequence A, B, C with some
lucinations
[77].
The fact that hallucinations can occur
overlap. Those shown in Ad have persisted for several years and
in other sensory modalities in the absence of psychi-may be generated in the lateral geniculate nucleus where
atric involvement suggests that the term “CBS” might
reinnervation may occur less readily. (From
[60],
with permission.)
reasonably be applied to these occurrences also but this
is not the case at present.
in the highest regions. However, the evidence to date
Hallucinations could depend on a purely excita-
does not support this idea
[66, 67].
It may be that the
tory effect or there could be removal of a maintained
progression through the visual cortex from simple to
inhibition, a “disinhibition.” Cogan
[35]
classified
complex is dependent on the ability of the cortical neu-visual hallucinations into “irritative” and “release.”
rons to emit marked spontaneous discharges, and this
The former were compared to an “epileptic” or “ictal”
ability would vary in different individuals.
attack, whereas the latter was presumably a disinhibition. In fact, we do not usually have enough information to decide between these two alternatives or even
Theories of hallucination generation
to determine if they are alternatives. For convenience, I
There are two broad theories of hallucination genera-will concentrate on the purely excitatory model, always
tion
[68].
The first theory, the “Perception and Atten-remembering that other possibilities exist.
tion Deficit Model”
[69]
, proposes that there is both
Several synapses, some from the mammalian cen-
impaired attention and poor sensory activation and
tral nervous system, some from elsewhere, have been
the interaction between the two leads to hallucina-
studied in great detail under conditions in which the
tions. This model may be appropriate for the hallucina-inputs have been varied widely. There has been a large
tions of schizophrenia and some other hallucinations,
measure of agreement between the different reports.
although a case has been made out for a deafferentation
Total silencing of the input to a synapse leads to the
model here also
[70].
The second model emphasizes
following presynaptic changes: increases in the size of
372
the “deafferentation syndrome” aspect
[18,
68, 71].
It
the terminal bouton, in the total number of vesicles, in
Chapter 30 – The Charles Bonnet Syndrome
Table 30.1
Cortical areas with increased sensitivity to specific visual stimuli
Name of area
Acronym
Anatomy
Stimulus/function
Reference
Fusiform face area
FFA
Fusiform gyrus
Faces
Kanwisher et al., 1997 [84]
Parahippocampal place
PPA
Parahippocampal gyrus
Scenery
Epstein and Kanwisher, 1998 [85]
area
Superior temporal
STS-FA
Superior temporal sulcus
Movements of the
Perrett et al., 1982, 1995 [86, 87]
sulcus face area
eyes and mouth
Puce et al., 1998 [88]
Extrastriate body area
EBA
Lateral occipitotemporal
Whole body
Downing et al., 2001 [89]
cortex
Lateral occipital
LOC
Lateral and ventral occipital
Analysis of object
Kourtzi and Kanwisher, 2000 [90]
complex
cortex
structure
Visual word form area
VWFA
Left ventral occipitotemporal
Text
Cohen and Dehaene, 2004 [91]
sulcus
the number of docked vesicles, in the size of the release
parahippocampal gyri in the conscious patient causes
zone, in the size of the readily releasable pool, and
an awakening of memories of people, animals, and
in the release probability
[72].
Postsynaptically silenc-scenes
[42].
ing of the synapse causes “externalization” of synap-Second, functional magnetic resonance imag-
tic receptors that become “internalized” when synap-
ing (fMRI) from hallucinating patients has revealed
tic traffic increases
[79, 80, 81, 82].
The postsynaptic
increased activity in ventral temporal lobe, with one
membrane also shows greater electric excitability dur-patients hallucinating faces showing heightened activ-ing disuse of the synapse
[65].
All of these changes
ity in the fusiform gyrus of the ventral occipital lobe
point in the same direction: increased excitability
of the synapse during deafferentation. In certain
Lastly, in this general region, several areas have
conditions, this may lead to increased spontaneous
been delineated as containing neurons with increased
activity.
sensitivity to specific visual stimuli
(Table 30.1).
These
Most neurons in the visual system are binocu-
areas have been mapped using fMRI or positron emis-
lar. Therefore, these are deafferented only when the
sion tomography (PET) technology or direct recording
inputs from the corresponding parts of both eyes are
from individual neurons.
lost. However, most neurons in the lateral geniculate
The FFA seems to be the same as the area men-
nucleus are monocular, and in cortical area V1, there
tioned in the last-but-one paragraph and is probably
are monocular neurons activated only from contralat-
concerned with facial recognition, whereas the STS-
eral nasal retina. Before the extent of deafferentation
FA is more related to facial expression
[92].
The areas
can be judged, it is necessary to have a detailed knowl-described by Wicker and colleagues
[93]
as concerned
edge of the position and size of the lesion. This is sel-with gaze would have included STS-FA. Lesion of the
dom possible. When the damage is in the cerebral cor-VWFA causes alexia but may also lead to VHs con-
tex, the more anterior the lesion, the less likely will
sisting of grammatically correct, meaningful written
there be any hallucinations
[63];
this may be because
sentences or phrases
[94].
The patient cannot read but
the chance of deafferentation is less.
can hear and write correctly what she hears. There is
evidently an area in this region deafferented by the
Site of complex hallucinations
lesion in the VWFA, possibly the anterior fusiform
There is now evidence from separate types of study
area described by Nobre and colleagues
[95]
or part
strongly suggesting that complex VHs are generated
of the cortical area associated with auditory hallucina-in visual areas in the temporal lobe of the cerebral
tions because of the resemblance of the hallucinations
cortex and some adjacent regions. The evidence is
to those experienced by schizophrenics
[94].
threefold. First, electrical stimulation of the ven-
The conclusion from these three separate
tral superior, middle, and inferior temporal gyri; of
approaches is that complex VHs are closely asso-
373
the inferior parietal lobule; and of the fusiform and
ciated with increased activity in a region of cortex
Related Concepts – Section 4
extending from superior temporal cortex ventrally to
Prevalence and incidence
the parahippocampal gyrus and probably originate in
The published estimates are unreliable for several
one or other part of this region. There is no reason why
reasons:
this conclusion should not apply to all VHs, whatever
their etiology. However, each patient has a unique
1. There is no agreed definition of CBS.
pattern of hallucinations and it is not surprising that
2. The available data are derived from highly selected
these differ from the images created by the highly
populations of patients, for example,
abnormal electrical stimulation of the brain or from
ophthalmology clinics.
mental imagery
[52].
The view presented here is
3. Patients experiencing complex hallucinations may
radically different from that of Weinberger and Grant
not report them for fear of being treated as insane.