SM 101: A Realistic Introduction (68 page)
Read SM 101: A Realistic Introduction Online
Authors: Jay Wiseman

Furthermore, and my
biggest
concern, I know of no reliable way to determine when such a cardiac arrest has become imminent. Often the first detectable sign that an arrest is approaching is the arrest itself. Furthermore, if the recipient does arrest, the probability of resuscitating them, even with optimal CPR, is distinctly small. Thus the recipient is dead and their partner, if any, is in a very perilous legal situation. (The authorities could consider such deaths first-degree murders until proven otherwise, with the burden of such proof being on the defendant).
There are also the real and maj or concerns of the surviving partner’s own lifelong remorse about having caused such a death, and the trauma to the friends and family members of both parties.
Some breath control fans say that what they do is acceptably safe because they do not take what they do up to the point of unconsciousness. I find this statement a bit worrisome for two reasons: (1) You can’t really know when a person is about to go unconscious until they actually do so, thus it’s extremely difficult to know where the actual point of unconsciousness is until you actually reach it. (2) More importantly, unconsciousness is a symptom, not a condition in and of itself. It can have underlying causes ranging from simple fainting to cardiac arrest, and which of these will cause the unconsciousness cannot be known in advance.
I have discussed my concerns regarding breath control with well over a dozen SM-positive physicians, and with numerous other SM-positive health professionals, and all share my concerns. We have discussed how breath control might be done in a way that is not life-threatening, and come up blank. We have discussed how the risk might be significantly reduced, and come up blank. We have discussed how it might be determined that an arrest is imminent, and come up blank. Indeed, so far not one (repeat, not one) single physician, nurse, paramedic, chiropractor, physiologist, or other person with substantial training in how a human body works has been willing to step forth and teach a form of breath control play that they are willing to assert is acceptably safe- i.e., does not put the recipient at imminent risk of dying. I believe this fact makes a major statement.
Other “edge play” topics such as suspension bondage, electricity play, cutting, piercing, branding, enemas, water sports, and scat play can and have been taught with reasonable safety, but not breath control play. Indeed, it seems that the more somebody knows about how a human body works, the more likely they are to caution people about how dangerous breath control is, and about how little can be done to reduce the degree of risk.
In many ways, oxygen is to the human body, and particularly to the heart and brain, what oil is to a car’s engine. Indeed, there’s a medical adage that goes “hypoxia (becoming dangerously low on oxygen) not only stops the motor, but also wrecks the engine.” Therefore, asking how one can play safely with breath control is very similar to asking how one can drive a car safely while draining it of oil. Some people tell the “mechanics” something like, “Well, I’m going to drain my car of oil anyway, and I’m not going to keep track of how low the oil level is getting while I’m driving my car, so tell me how to do this with as much safety as possible.” They then get frustrated when the mechanics scratch their heads and say that they don’t know. They may even label such mechanics as “anti-education.”
A bit about my background may help explain my concerns. During my ambulance days, I responded to at least one call involving the death of a young teenage boy who died from autoerotic strangulation, and to several other calls where this was suspected but could not be confirmed. (Family members often “sanitize” such scenes before calling 911.) Additionally, I personally know two members of my local SM community who went to prison after their partners died during breath control play.
The primary danger of suffocation play is that it is not a condition that gets worse over time (regarding the heart, anyway; it does get worse over time regarding the brain). Rather, what happens is that the more the play is prolonged, the greater the odds that a cardiac arrest will occur. Sometimes even one minute of suffocation can cause this; sometimes even less.
Quick pathophysiology lesson #1: When the heart gets low on oxygen, it starts to fire off “extra” pacemaker sites. These usually appear in the ventricles and are thus called premature ventricular contractions - PVCs for short. If a PVC happens to fire off during the electrical repolarization phase of cardiac contraction (the dreaded “PVC on T” phenomenon, also sometimes called “R on T”) it can kick the heart over into ventricular fibrillation - a form of cardiac arrest. The lower the heart gets on oxygen, the more PVCs it generates, and the more vulnerable to their effect it becomes, thus hypoxia increases both the probability of a PVC-on-T occurring and of its causing a cardiac arrest. When this will happen to a particular person in a particular session is simply not predictable. This is exactly where most of the medical people I have discussed this topic with “hit the wall.”
Virtually all medical folks know that PVCs are both life-threatening and hard to detect unless the patient is hooked to a cardiac monitor. When medical folks discuss breath control play, the question quickly becomes: How can you know when they start throwing PVCs? The answer is: You basically can’t.
Quick pathophysiology lesson #2: When breathing is restricted, the body cannot eliminate carbon dioxide as it should, and the amount of carbon dioxide in the blood increases. Carbon dioxide (CO2) and water (H2O) exist in equilibrium with what’s called carbonic add (H2CO3) in a reaction catalyzed by an enzyme called carbonic anhydrase. Thus: CO2 + H20
Quick pathophysiology lesson #3: Again, if breathing is restricted, not only does carbon dioxide have a hard time getting out, but oxygen also has a hard time getting in. A molecule of glucose breaks down within the cell into two molecules of an acid called pyruvate, thus creating a small amount of ATP for the body to use as energy. Under normal circumstances, pyruvate quickly combines with oxygen to produce a much larger amount of ATP. However, if there’s not enough oxygen to properly metabolize the acidic pyruvate, it builds up and produces one form of what’s called a metabolic acidosis. As you can see, either a build-up in the blood of carbon dioxide or a decrease in the blood of oxygen will cause the pH of the blood to fall. If both occur at the same time, as they do in cases of suffocation, the pH of the blood will plummet to life-thteatening levels within a very few minutes. The pH of normal human blood is in the 7.35 to 7.45 range (slightly alkaline). A pH falling to 6.9 (or raising to 7.8) is “incompatible with life.” Past experience, either with others or with that same person, is not particularly useful. Carefully watching their level of consciousness, skin color, and pulse rate is of only limited value. Even hooking the bottom up to both a pulse oximeter and a cardiac monitor (assuming you had either piece of equipment, and they’re not cheap) would be of only limited additional value. While an experienced clinician can sometimes detect PVCs by feeling the patient’s pulse, in reality the only reliable way to detect them is to hook the patient up to a cardiac monitor. The problem is that each PVC is potentially lethal, particularly if the heart is low on oxygen. Even if you “ease up” on the bottom immediately, there’s no telling when the PVCs will stop. They could stop almost at once, or they could continue for hours.
In addition to the primary danger of cardiac arrest, there is good evidence to document that there is a very real risk of cumulative brain damage if the practice is repeated often enough. In particular, laboratory studies of repeated brief interruption of blood flow to the brains of animals and studies of people with what’s called “sleep apnea syndrome” (in which they stop breathing for up to two minutes while sleeping) document that cumulative brain damage does occur in such cases. There are many documented additional dangers. These include, but are
not
limited to: rupture of the windpipe, fracture of the larynx, damage to the blood vessels in the neck, dislodging a fatty plaque in a neck artery which then travels to the brain and causes a stroke, damage to the cervical spine, seizures, airway obstruction by the tongue, and aspiration ofvomitus. Additionally, there are documented cases in which the recipient appeared to fully recover but was found dead several hours later. The American Psychiatric Association estimates a death rate of one person per year per million of population - thus about 250 deaths last year in the U.S. Law enforcement estimates go as much as four times higher.
Most such deaths occur during solo play, however there are many documented cases of deaths that occurred during play with a partner. It should be noted that the presence of a partner does nothing to limit the primary danger, and does little or nothing to limit most of the secondary dangers.
Some people teach that choking can be safely done if pressure on the windpipe is avoided. Their belief is that pressing on the arteries leading to the brain while avoiding pressure on the windpipe can safely cause unconsciousness. The reality, unfortunately, is that pressing on the carotid arteries,
exactly
as they recommend, presses on baroreceptors known as the carotid sinus bodies. These bodies then cause vasodilation in the brain; thus, there is not enough blood to perfuse the brain and the recipient loses consciousness. However, that’s not the whole story.
Unfortunately, a message is also sent to the main pacemaker of the heart, via the vagus nerve, to decrease the rate and force of the heartbeat. Most of the time, under strong vagal influence, the rate and force of the heartbeat decreases by one third. However, every now and then, the rate and force decreases to zero and the bottom “flatlines” into asystole - another, and more difficult to cope with, form of cardiac arrest. There is no way to tell whether or not this will happen in any particular instance, or how quickly. There are many documented cases of as little as five seconds of choking causing a vagal-outflow-induced cardiac arrest.
For thereason cited above, many police departments have noweither entirely banned the use of choke holds or have reclassified them as a form of deadly force. Indeed, a local CHP officer recently had a $250,000 judgment brought against him after a nonviolent suspect died while being choked by him.
Finally, as a CPR instructor myself, I want to caution that knowing CPR does little to make the risk of death from breath control play significantly smaller. While CPRcan andshould be done, understand that the probability of success is likely to be less than 10%.
I’m not going to state that breath control is something that nobody should ever do under any circumstances. I have no problem with informed, freely consenting people taking any degree of risk they wish. I am going to state that there is a great deal of ignorance regarding what actually happens to a body when it’s suffocated or strangled, and that the actual degree of risk associated with these practices is far greater than most people believe. I have noticed that, when people are educated regarding the severity and unpredictability of the risks, fewer and fewer choose to play in this area, and those who do continue tend to play less often. I also notice that, because of its severe and unpredictable risks, more and more SM partygivers are banning any form of breath control play at their events.
If you’d like to look into this matter further, here are some references to get you started: “Medical Physiology” by Guyton; “Emergency Care in the Streets” by Caroline; “The Pathologic Basis of Disease” by Robbins; “Textbook of Advanced Cardiac Life Support” by American Heart Association; “Forensic Pathology” by DeMaio and Demaio; “Autoerotic Fatalities” by Hazelwood; Journal of Forensic Sciences. People with questions or comments can contact me at [email protected] or write to me at P.O. Box 1261, Berkeley, CA 94701.
OTHER BOOKS FROM GREENERY PRESS
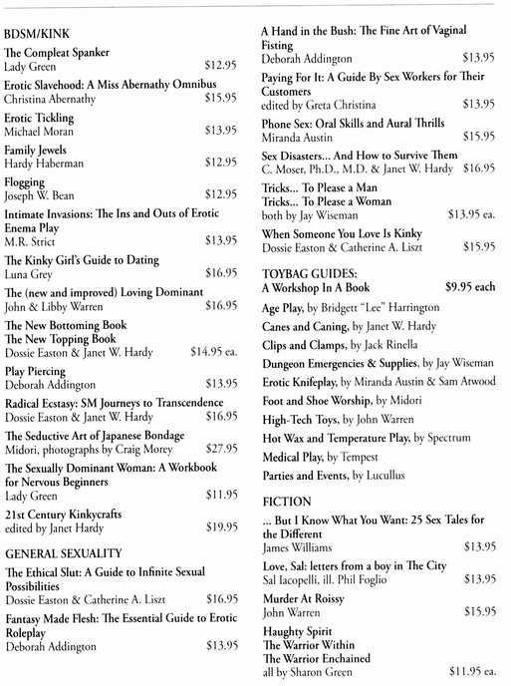
Please include $3 for first book and $1 for each additional book with your order to cover shipping
and handling costs, plus $10 for overseas orders. VISA, MC, AmEx & Discover accepted. Order
from Greenery Press, 4200 Park Blvd. pmb 240, Oakland, CA 510/530-1281.
Table of Contents