Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (133 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

Imaging studies
: Ultrasonography is useful for detecting the presence of ascites as well as for determining the etiology. It may reveal evidence of chronic liver disease, malignancy, hepatomegaly, and pancreatic disorder.
Ascites fluid findings
: AF examination is the principle diagnostic tool. Using abdominal paracentesis to obtain and study the fluid is crucial to making a diagnosis.

Transparent to pale fluid
: Is seen in cases of portal hypertension. Neutrophilia in excess of 1,000/mL results in opalescence. A concentration of RBCs in excess of 10,000/mL gives a faint pink tinge, and cell counts >20,000/mL color it red. A traumatic tap is evident by a streak of blood rather than homogeneously red fluid and the tendency to clot. Hepatocellular carcinoma and, rarely, metastatic disease; can cause a bloody tap. TB is only a rare cause of hemorrhagic ascites.

Chylous or milky ascites
: Has a higher triglyceride concentration than serum and >200 mg/dL. It is rarely seen and is usually an indication of cirrhosis rather than lymphoma or TB as was previously thought. The triglycerides are >1,000 mg/dL in truly milky ascites. Dark-brown ascites may be seen in significant hyperbilirubinemia, biliary perforation (when ascitic bilirubin is higher than serum bilirubin), pancreatitis, and, rarely, in malignant melanoma.

Bloody ascites fluid
: Once a traumatic tap has been ruled out, 50% of cases are due to hepatocellular carcinoma. TB rarely causes bloody fluid.

Staining
: Gram staining has low yield. Even with centrifugation, it has 10% sensitivity in spontaneous bacterial peritonitis. AFB smear for TB have very low sensitivity. In an appropriate clinical setting of low-grade fever, malaise, and weight loss, a high cell count with lymphocytic predominance and low SAAG is suggestive of TB ascites.

Protein concentration
of AF categorized ascites into exudative (ascitic protein >2.5 g/dL) or transudative (ascitic protein <2.5 g/dL). The significance of this has never been evaluated adequately and objectively.

Cell count and differential
: In uncomplicated cirrhosis, the total WBC count is <500 cells/μL with <250 neutrophils/μL. After diuresis, the total cell count may go up, but the neutrophil count remains below 250 cells/μL. In spontaneous bacterial peritonitis, the total WBC count and neutrophil count are usually, but not always, raised. In TB and carcinomatosis, the cell count rises but with a predominance of lymphocytes. In traumatic taps, for every 250 RBCs, one neutrophil is subtracted from the total WBC count.
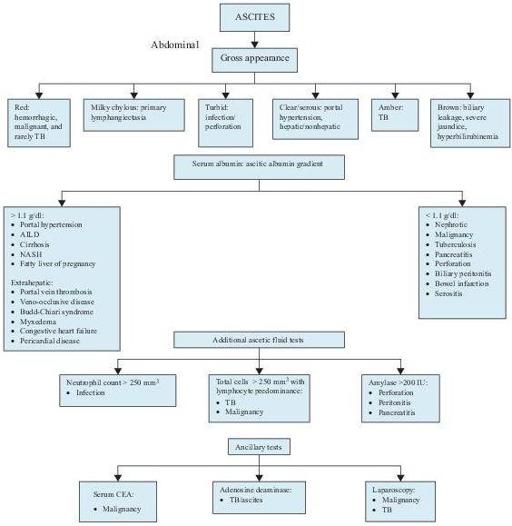
Figure 5–2
Algorithm for the workup of patients with ascites. AILD, alcohol-induced liver disease; CEA, carcinogenic embryonic antigen; NASH, nonalcoholic steatohepatitis; TB, tuberculosis; TNC, total neutrophil count.
Core laboratory
: The serum and AF glucose concentrations are nearly the same in uncomplicated portal hypertension (large numbers of WBCs, bacteria, or tumor cells consume glucose and may lead to diminished levels). Amylase values may be about 3–5 times higher than the serum values. LD levels rise because of release of LD from the neutrophils. The rise occurs in cases of secondary peritonitis, TB, and pancreatitis.
Cytology
: Has limitations in the diagnosis of malignant ascites and has been replaced largely laparoscopic examination of the peritoneum along with biopsy and culture.
Limitations
Errors may occur if serum albumin is very low or when serum and ascitic samples are not obtained within a short space of time from each other.
A high globulin level in serum may also give a false result.
DISORDERS OF THE PERITONEUM ASSOCIATED WITH ASCITES
CHRONIC LIVER DISEASE (SEE P. 198)
This disease differs from ascites caused by malignancy.