Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (209 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

Serum T
3
is usually elevated with hyperthyroidism. Assessment of T
3
levels is important to determine the severity of the hyperthyroidism and to monitor the response to treatment.
RAIU is often elevated in Graves disease. However, the diagnostic accuracy of RAIU in hyperthyroidism does not approach that of the serum TSH plus free T
4
measurement. Therefore, determining RAIU is not useful in the diagnosis of straightforward Graves disease but is useful in excluding thyrotoxicosis not caused by hyperthyroidism. Very low values of RAIU in association with thyrotoxicosis signal the presence of factitious thyrotoxicosis, ectopic thyroid tissue, subacute thyroiditis, or the thyrotoxic phase of autoimmune thyroiditis.
Thyrotropin receptor autoantibodies are present in 70–100% of the patients with Graves disease, and their measurement is not usually necessary for diagnosis, but it may be helpful in prognosis because patients who have high titers that do not decrease with antithyroid drug treatment are unlikely to go into remission. Measurement of thyrotropin receptor autoantibodies is important in pregnancy, because a high titer at the end of pregnancy correlates with an increased risk of neonatal hyperthyroidism.
Abnormal TSH can also been seen in various nonthyroidal diseases. Simultaneous measurement of TSH with free T
4
is useful in evaluating the differential diagnoses.
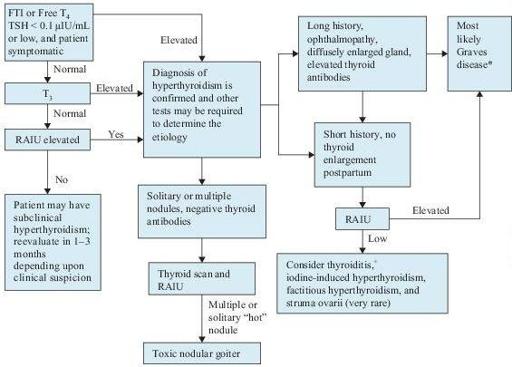
Figure 6–1
Algorithm for the diagnosis of hyperthyroidism. *Graves disease can be confirmed by measuring thyroid antibodies.
+
Suspect postpartum thyroiditis if within 6 months of delivery, subacute thyroid if associated with tender gland and constitutional symptoms, and silent thyroiditis if neither. T
4
, thyroxine; FTI, free thyroxine index; RAIU, radioactive iodine uptake; T
3
, triiodothyronine; TSH, thyroidstimulating hormone.
Suggested Readings
Khan F, Sachs H, Pechet L, et al.
Guide to Diagnostic Testing
. Philadelphia, PA: Lippincott Williams & Wilkins; 2002.
Kronenberg HM, Melmed S, Polonsky KS, et al.
Williams Textbook of Endocrinology
, 11th ed. Philadelphia, PA: Saunders, Elsevier Inc., 2008.
Ross DS. Diagnosis of hyperthyroidism. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Ross DS. Overview of the clinical manifestations of hyperthyroidism in adults. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
HYPOTHYROIDISM
Definition
Hypothyroidism refers to a condition in which the amount of thyroid hormones in the body is below normal.
Overview
The diagnosis of hypothyroidism relies heavily upon laboratory tests because of the lack of specificity of the typical clinical manifestations. The prevalence of hypothyroidism is approximately 5% in adults and 15% in women older than 65 years of age. Hypothyroidism is less common in men, with a five to eight times lower incidence. Hypothyroidism is far more common than hyperthyroidism. Hypothyroidism is usually easily treated with thyroid hormone replacement. It is now hypothesized that autoimmune hyperthyroidism (Graves disease) and hypothyroidism (Hashimoto thyroiditis) represent two extremes of one spectrum of autoimmune thyroid disease.
Common Causes
I. Primary hypothyroidism
A. Hashimoto thyroiditis is the most common cause of hypothyroidism in areas of the world in which dietary iodine is sufficient. It usually presents with goiter, hypothyroidism, or both. Goiter usually develops gradually. The diagnosis of Hashimoto thyroiditis is confirmed by the presence of thyroid autoantibodies, including thyroid peroxidase (TPO) antibody and thyroglobulin antibody.
B. Iatrogenic: Thyroidectomy and radioiodine therapy or external irradiation for the treatment of carcinoma, hyperthyroidism, or goiter can lead to hypothyroidism.
C. Iodine deficiency (endemic goiter) almost always occurs in areas of environmental iodine deficiency. The incidence of endemic goiter has been greatly reduced by the introduction of iodized salt.
D. Drugs: thioamides, lithium, amiodarone, interferon, and interleukin-2
E. Infiltrative diseases such as fibrous thyroiditis, hemochromatosis, and sarcoidosis
F. Transient hypothyroidism is defined as a period of reduced free T
4
with suppressed, normal, or elevated TSH levels that are eventually followed by an euthyroid state. This form of hypothyroidism usually occurs in the clinical context of subacute (postviral) thyroiditis, lymphocytic (painless) thyroiditis, or postpartum thyroiditis
G. Congenital thyroid agenesis, dysgenesis, or defect in hormone synthesis
H. Subclinical hypothyroidism is defined as a normal serum free T
4
concentration and a slightly high serum TSH concentration. These patients usually have nonspecific symptoms and a substantial proportion of them eventually develop overt hypothyroidism
II. Secondary and tertiary (central) hypothyroidism refers to hypothyroidism induced by deficiency of either TSH or thyrotropin-releasing hormone (TRH). This type of hypothyroidism is much less common than primary hypothyroidism, and the symptoms are usually milder than in primary hypothyroidism.