Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (213 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

D. Midnight serum cortisol is based on the fact that the normal evening or night nadir in serum cortisol is preserved in obese and depressed patients (pseudo-Cushing syndrome) but not in those with Cushing syndrome. The test needs to be repeated on at least two nights. Accuracy of midnight cortisol requires an indwelling catheter, and it is clearly not convenient in an outpatient setting.
III. Tests used to localize the source of the hormone excess: Once the diagnosis of Cushing syndrome is confirmed, the next step is to distinguish among the three most common causes: a pituitary tumor, ectopic ACTH secretion, and an adrenal tumor. Determining whether elevated cortisol is ACTH dependent (due to an ACTH-secreting tumor) or whether it is ACTH independent (due to a primary adrenal disorder) is based primarily on measuring plasma ACTH level.
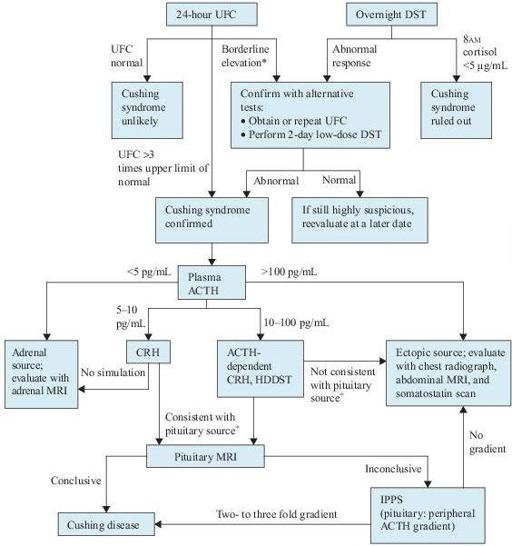
Figure 6–4
Algorithm for the evaluation of Cushing syndrome. *Patients with alcoholism or depression may have pseudo-Cushing syndrome and require a CRH test for further evaluation.
+
With a pituitary source, ACTH should increase with CRH, and cortisol production should decrease with HDDST. ACTH, adrenocorticotropic hormone; CRH, corticotropin-releasing hormone; DST, dexamethasone suppression test; HDDST, high-dose dexamethasone suppression test; MRI, magnetic resonance imaging; IPPS, inferior petrosal sinus sampling; UFC, urinary free cortisol.
TABLE 6–2. Common Tests Used to Establish the Diagnosis of Cushing Syndrome
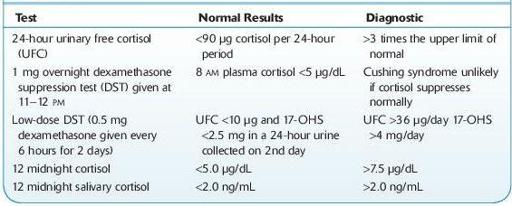
17-OHS, 17-hydroxycorticosteroid.
Imaging Studies (see Figure
6-4
)
1. Adrenal imaging is indicated when plasma ACTH levels are <5 pg/mL. Thinsection CT or MRI is the next step in evaluating the adrenals. Bilateral adrenal hyperplasia may be present in ACTH-dependent disease.
2. Somatostatin scanning. Ectopic sources of ACTH are notoriously difficult to identify. Because many of these tumors are carcinoids and have somatostatin receptors, scintigraphy with the somatostatin analog indium-111-pentreotide can sometimes localize tumors not found by conventional techniques.
3. Because both incidental pituitary and adrenal tumors are common, biochemical evaluation should be completed before any imaging studies.
Additional Study
Petrosal sinus sampling is used when the anatomic localization fails to identify an unequivocal lesion as suggested by the biochemical testing. This test allows confirmation of the pituitary source of ACTH and identifies the side of the ACTHsecreting lesion. ACTH is measured simultaneously in samples from catheters placed in the left and right inferior petrosal sinuses and compared to peripheral levels. A gradient of two- to threefold is consistent with a pituitary source of ACTH. CRH can also be given during the procedure to enhance its accuracy.
Suggested Readings
Khan F, Sachs H, Pechet L, et al.
Guide to Diagnostic Testing
. Philadelphia, PA: Lippincott Williams & Wilkins; 2002.
Kronenberg HM, Melmed S, Polonsky KS, et al.
Williams Textbook of Endocrinology
, 11th ed. Philadelphia, PA: Saunders, Elsevier Inc.; 2008.
Nieman LK. Causes and pathophysiology of Cushing’s syndrome. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Nieman LK. Clinical manifestations of Cushing’s syndrome. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Nieman LK. Establishing the cause of Cushing’s syndrome. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Nieman LK. Establishing the diagnosis of Cushing’s syndrome. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
ADRENAL INSUFFICIENCY
Definition
Adrenal insufficiency is defined as a deficiency of hormones synthesized by the adrenal cortex.
Common Causes
I. Primary adrenal insufficiency (Addison disease): due to intrinsic diseases of the adrenal glands
A. Autoimmune adrenalitis. It is the most common cause of primary adrenal insufficiency and comprises approximately 70–80% of the cases. Some of the patients also have other autoimmune disorders, such as hypoparathyroidism, type 1 DM, Hashimoto thyroiditis, Graves disease, or pernicious anemia.
B. Infections. Common infectious etiologies include tuberculosis, fungi (histoplasmosis, paracoccidioidomycosis), bacteria (meningococcemia,
Pseudomonas aeruginosa
), and viruses (HIV, CMV).
C. Adrenal hemorrhage or infarction. Adrenal hemorrhage has been associated with meningococcemia (Waterhouse-Friderichsen syndrome) or
Pseudomonas aeruginosa
. Anticoagulants are a major risk factor for adrenal hemorrhage.
D. Metastatic disease. Infiltration of the adrenal glands by metastatic cancers is common. The primary site includes the lung, breast, stomach, and colon. Similar findings can be seen with melanomas or lymphomas.
E. Drugs. Several drugs may cause adrenal insufficiency by inhibiting cortisol biosynthesis. They include etomidate, ketoconazole, metyrapone, and suramin.
F. Other risk factors include antiphospholipid syndrome, thromboembolic disease, trauma, stress, adrenoleukodystrophy, and abetalipoproteinemia.
II. Secondary adrenal insufficiency: due to inadequate ACTH secretion by the pituitary
A. Panhypopituitarism. Symptoms are due to a decrease in all pituitary hormones, resulting in hypoadrenalism.
B. Isolated ACTH deficiency.
C. Megestrol acetate. Megestrol is used as an appetite stimulant in patients with metastatic breast cancer or AIDS. It suppresses the hypothalamic–pituitary–adrenal axis.
III. Tertiary adrenal insufficiency: due to inadequate CRH secretion by the hypothalamus
A. Following abrupt cessation of high-dose glucocorticoid therapy
B. Following correction of Cushing syndrome
Who Should Be Suspected?