Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (214 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

Clinical symptoms and signs of adrenal insufficiency vary depending on the rate and extent of loss of adrenal function, whether mineralocorticoid production is preserved, and the degree of stress.
1. Adrenal crisis. It refers to acute adrenal insufficiency, and the predominant manifestation is shock. Other symptoms include anorexia, nausea, vomiting, abdominal pain, weakness, fatigue, lethargy, confusion, or coma. Adrenal crisis may occur in patients with gradual onset who have been stressed by infection, trauma, or surgery.
2. The most common symptoms of chronic adrenal insufficiency are chronic malaise, anorexia, nausea, vomiting, and generalized weakness.
3. Patients with long-standing primary adrenal insufficiency may present with hyperpigmentation. Other frequent signs are hypotension or orthostatic hypotension. Calcification of the auricular cartilage occurs exclusively in men.
4. Patients with secondary and tertiary adrenal insufficiency usually have intact mineralocorticoid function and do not develop hyponatremia and/or hyperkalemia.
Laboratory Findings (Figure
6-5
)
1. Serum cortisol concentration. Cortisol is secreted in a diurnal pattern with highest levels in the morning. Levels measured later in the day are unreliable. Healthy people have early morning serum cortisol concentration of >15 μg/dL. Values <15 μg/dL are suggestive of adrenal insufficiency and require further testing.
2. Basal plasma ACTH concentration. An elevated morning ACTH plasma level in the presence of low cortisol is diagnostic of primary adrenal insufficiency. In contrast, plasma ACTH concentrations are low or low normal in secondary or tertiary adrenal insufficiency.
3. ACTH stimulation tests. If the diagnosis of adrenal insufficiency is being considered and the patients have early morning serum cortisol concentration <15 μg/ dL, a short ACTH stimulation test should be performed. A subnormal response confirms the diagnosis of adrenal insufficiency.
4. Corticotropin-releasing hormone test. Differentiation between secondary and tertiary adrenal insufficiency can be done by a corticotropin-releasing hormone test. Patients with secondary adrenal insufficiency show little or no ACTH response, whereas patients with tertiary disease usually have an exaggerated and prolonged ACTH response.
5. Antiadrenal antibodies. Antibodies against 21-hydroxylase (P450c21) are identified in 60–70% of patients with autoimmune adrenal insufficiency. They frequently precede the onset of disease. They are also present in 20% of patients with hypoparathyroidism.
6. Patients with suspected adrenal crisis should be treated with dexamethasone, which does not cross-react in the cortisol assay, and confirmatory tests should be performed within 1–2 days.
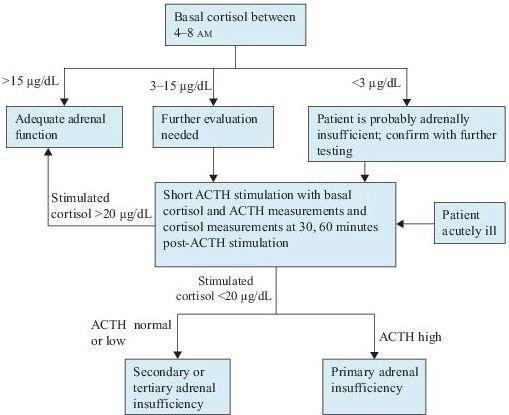
Figure 6–5
Algorithm for the diagnosis of adrenal insufficiency. ACTH, adrenocorticotropic hormone.
Imaging Studies
In patients with primary adrenal insufficiency, abdominal CT or MRI with specific attention to adrenals should be obtained to identify the etiology. Enlarged adrenals suggest infectious, hemorrhagic, or metastatic diseases. Pituitary CT or MRI should be performed to look for masses in patients with secondary or tertiary adrenal insufficiency.
Suggested Readings
Khan F, Sachs H, Pechet L, et al.
Guide to Diagnostic Testing
. Philadelphia, PA: Lippincott Williams & Wilkins; 2002.
Kronenberg HM, Melmed S, Polonsky KS, et al.
Williams Textbook of Endocrinology
, 11th ed. Philadelphia, PA: Saunders, Elsevier Inc.; 2008.
Nieman LK. Causes of primary adrenal insufficiency (Addison’s disease). In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Nieman LK. Causes of secondary and tertiary adrenal insufficiency in adults. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Nieman LK. Clinical manifestations of adrenal insufficiency in adults. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Nieman LK. Diagnosis of adrenal insufficiency in adults. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Nieman LK. Evaluation of the response to ACTH in adrenal insufficiency. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
PRIMARY HYPERALDOSTERONISM
Definition
Primary hyperaldosteronism is a syndrome characterized by hypertension, hypokalemia, and suppressed plasma renin activity associated with increased aldosterone excretion.
Common Causes
1. Aldosterone-producing adenoma accounts for 65% of the cases. Patients tend to have more severe hypertension, lower potassium levels, higher aldosterone secretion, and are of younger age than patients with idiopathic hyperaldosteronism. Unilateral adrenalectomy is curative.
2. Bilateral idiopathic hyperaldosteronism comprises approximately 20–30% of the cases. Bilateral hyperplasia is present.
3. Primary adrenal hyperplasia refers to unilateral aldosterone secretion in patients with physiologic changes similar to those of bilateral idiopathic hyperaldosteronism.
4. Aldosterone-producing adrenocortical carcinoma
5. Ectopic aldosterone-secreting tumors can be of ovarian or renal origin.
Who Should Be Suspected?
The classic presenting signs of primary aldosteronism are hypertension, hypokalemia, and edema.
1. Hypertension. The blood pressure in primary aldosteronism is often substantially elevated with mean values of 184/112 and 161/105 mm Hg in patients with adrenal adenoma and adrenal hyperplasia, respectively. However, malignant hypertension rarely occurs.
2. Hypokalemia. Potassium level is low with inappropriate potassium wasting. Plasma potassium tends to be relatively stable at least over the short-term as the potassium-wasting effect of excess aldosterone is counterbalanced by the potassium-retaining effect of hypokalemia itself. Progressive hypokalemia does not occur unless some other factor is added. Hypokalemia may not be the initial presentation, but it is a common finding after administration of diuretics such as furosemide.
3. Metabolic alkalosis
4. Peripheral edema
5. Hypomagnesemia
6. Muscle weakness
Laboratory Findings (Figure
6-6
)