Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (210 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

III. Generalized thyroid hormone resistance
Who Should Be Suspected?
Signs and symptoms of hypothyroidism include:
1. Fatigue, weight gain, depression, and cold intolerance
2. Dry skin, brittle hair, constipation, and muscle cramps
3. Hypermenorrhea in women
4. Thyroid enlargement (goiter), puffy face and hands (myxedema), and delayed ankle reflex relaxation phase
5. Hypothyroidism in infants and children leads to retardation of mental development and of growth. Severe hypothyroidism in infancy is termed cretinism.
6. Myxedema coma refers to severe prolonged hypothyroidism, which is manifested by bradycardia, congestive heart failure, hypothermia, hypoventilation, and paralytic ileus. It is an uncommon but life-threatening condition if not detected and treated promptly.
7. Secondary and tertiary hypothyroidism should be suspected in patients with known hypothalamic or pituitary disease, patients with a pituitary mass, or in patients with other hormonal deficiencies.
Laboratory Findings (Figure
6-2
)
Laboratory confirmation of the diagnosis of hypothyroidism consists of measuring serum TSH and free T
4
. Primary hypothyroidism is characterized by a high serum TSH concentration and a low serum free T
4
concentration. Secondary hypothyroidism is characterized by a low serum TSH concentration as well as a low serum T
4
concentration.
Total T
4
, RAIU, and free T
4
index are usually decreased in hypothyroidism, but they are less sensitive than TSH and free T
4
measurement.
Antithyroid peroxidase (TPO) antibodies are detected in almost all patients with Hashimoto disease and its variants, in 70% of patients with Graves disease, and in a smaller number of patients with various other thyroid disorders such as MNG, nontoxic goiter, and thyroid carcinoma.
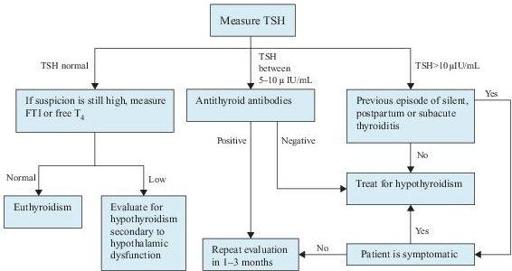
Figure 6–2
Algorithm for the diagnosis of hypothyroidism. T
4
, thyroxine; FTI, free thyroxine index; TSH, thyroid-stimulating hormone.
Suggested Readings
Khan F, Sachs H, Pechet L, et al.
Guide to Diagnostic Testing
. Philadelphia, PA: Lippincott Williams & Wilkins, 2002.
Kronenberg HM, Melmed S, Polonsky KS, et al.
Williams Textbook of Endocrinology
, 11th ed. Philadelphia, PA: Saunders, Elsevier Inc., 2008.
Ross DS. Diagnosis of and screening for hypothyroidism. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
Ross DS. Subclinical hypothyroidism. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.
GOITER AND THYROID NODULES
Definition
Goiter refers to an enlargement of the thyroid gland. It can be classified in different ways. Toxic goiter refers to goiter with hyperthyroidism. Nontoxic goiter refers to an enlarged thyroid gland with normal or low thyroid hormone levels.
A thyroid nodule is defined as a discrete lesion within the thyroid gland that is due to an abnormal focal growth of thyroid cells.
Overview
Thyroid enlargement or nodules come to clinical attention when noted by the patient, or as an incidental finding during routine physical examination, or during a radiologic procedure, such as carotid ultrasonography or neck computed tomography (CT).
The prevalence of goiter, diffuse or nodular, differs widely depending on the iodine intake by the population living in a given area. In the general population, prevalence of 4.6% has been reported as being clinically detected. By using ultrasound as a screening method, a prevalence of up to 30–50% of an unselected adult population has been described as having goiter.
The clinical importance of thyroid nodules is related primarily to the need to exclude thyroid cancer, which accounts for 4–6.5% of all thyroid nodules in non-surgical series. The diagnostic goal is to efficiently identify those patients who require surgical intervention. A solitary nodule should be evaluated for malignancy no matter what the underlying thyroid disorder is.
Common Causes
I. Diffuse enlargement of the thyroid gland is seen in the following conditions:
Diffuse toxic goiter—Graves disease; most common cause of endogenous hyperthyroidism