Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis (218 page)
Authors: Mary A. Williamson Mt(ascp) Phd,L. Michael Snyder Md

6. Hypertension and diabetes
7. Onset of hypertension at young age (<20 years)
8. History of gastric stromal tumor or pulmonary chondroma (Carney triad)
Laboratory Findings (Figure
6-8
)
Evaluation includes analysis of plasma or urinary catecholamine and their metabolites. The diagnosis is typically confirmed by measurements of urinary and plasma fractionated metanephrines and catecholamines.
1. Twenty-four–hour urine catecholamines and metanephrines. It is traditionally relied upon by many institutions for the diagnosis of pheochromocytomas. Sensitivity and specificity of this test are approximately 98%. Measurement of urinary creatine should also be included to verify an adequate urine collection. A positive test is considered to be twofold elevation above the upper limit of normal in urine catecholamines or metanephrines.
2. Fractionated plasma free metanephrines. Some groups have advocated that fractionated plasma free metanephrines should be a first-line test for pheochromocytoma. The sensitivity of this test is 96–100%, and the specificity is approximately 85–89%. Therefore, the predictive value of a negative test is extremely high.
3. Patients must be off all interfering medications before urine or plasma catecholamines can be measured. Levels can be increased by tricyclic antidepressants, labetalol, levodopa, decongestants, amphetamines, ethanol, and benzodiazepines. Levels can be decreased by metyrosine and methylglucamine, which are present in contrast media. Patients should avoid acetaminophen (Tylenol) during the sample collection.
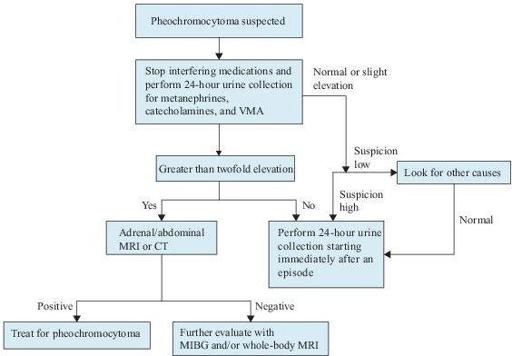
Figure 6–8
Algorithm for the diagnosis of pheochromocytoma. CT, computed tomography; MIBG, [
123
I]–metaiodobenzylguanidine; MRI, magnetic resonance imaging; VMA, vanillylmandelic acid.
Imaging Studies
1. CT and MRI will detect most sporadic tumors because they are usually larger than 3 cm in greatest dimension. MRI has some advantage, since pheochromocytomas have a typical hyperintense appearance on T2-weighted images.
2. [
123
I]-metaiodobenzylguanidine (MIBG) scintigraphy is useful in patients with negative CT or MRI.
Suggested Readings
Khan F, Sachs H, Pechet L, et al.
Guide to Diagnostic Testing
. Philadelphia, PA: Lippincott Williams & Wilkins; 2002.
Kronenberg HM, Melmed S, Polonsky KS, et al.
Williams Textbook of Endocrinology
, 11th ed. Philadelphia, PA: Saunders, Elsevier Inc.; 2008.
Young WF, Jr, Kaplan NM. Clinical presentation and diagnosis of pheochromocytoma. In: Rose B, (ed).
UpToDate
, Waltham, MA: UpToDate, Inc.; 2009.

GONADAL DISORDERS
GYNECOMASTIA
Definition
Gynecomastia is defined as excess development of male mammary tissue.
Overview
Gynecomastia is common in infancy, adolescence, and in middle-aged to elderly men. It may be present unilaterally or bilaterally. Gynecomastia develops in response to a variety of causes. The common mechanism of gynecomastia includes an imbalance between the stimulatory effects of estrogens (estradiol, estrone) and the inhibitory effects of androgens (testosterone, androstenedione). Any conditions that alter this balance, including increased production of estrogen, decreased production of androgen, or increased availability of estrogen precursors for peripheral conversion to estrogen, can lead to the proliferation of breast tissue.
Common Causes
Physiologic gynecomastia can occur in neonates and adolescents and usually resolves spontaneously in most cases. The most common causes seen in clinical practice in adult patients includes idiopathic (approximately 25%), persistent postpubertal (approximately 25%), drugs (approximately 10–25%), cirrhosis or malnutrition (approximately 8%), male hypogonadism (10%), testicular tumors (approximately 3%), hyperthyroidism (approximately 1.5%), and chronic renal failure (approximately 1%).
1. Idiopathic. Approximately 25% of the patients have no detectable abnormality. Gynecomastia can occur due to advanced age.
2. Persistent postpubertal gynecomastia. During puberty, serum estradiol concentrations rise to adult levels before the testosterone concentration. Pubertal gynecomastia usually resolves spontaneously within 6 months to 2 years of onset but in some instances may persist, leading to postpubertal gynecomastia. It is likely due to estrogen–androgen imbalance.
3. Drugs.
a. Androgen antagonists and inhibitors. For example, spironolactone, cimetidine, marijuana, flutamide, leuprolide, ketoconazole, finasteride, diazepam, tricyclic antidepressants, phenothiazines, alcohol, and chemotherapeutic agents
b. Estrogenic effects. For example, digitalis, diethylstilbestrol, marijuana, heroin, isoniazid, and alcohol
c. Increased availability of substrate or activity of aromatase. For example, exogenous administration of gonadotropins, testosterone, or phenytoin
d. Unknown mechanisms. For example, methyldopa, antihypertensives (ACE inhibitors, calcium channel blockers), narcotics, metronidazole, amiodarone, and omeprazole
4. Cirrhosis or malnutrition.
a. Gynecomastia can occur in up to 67% of cirrhotic patients. There are two mechanisms for this. First, the damaged hepatocytes have an impaired ability to clear androstenedione, which is then available for peripheral aromatase activity and subsequent conversion to estrogens. The second mechanism is through induction of sex hormone–binding globulin (SHBG). Because SHBG binds testosterone with greater affinity than estrogen, any condition that increases SHBG will alter the estrogen–androgen ratio in favor of estrogen.
b. Malnutrition. During starvation, gynecomastia can occur due to decreased gonadotropin and testosterone levels and normal estrogen production from adrenal precursors. Refeeding is associated with rising gonadotropin, resulting in increased testosterone secretion and marked elevated estrogen production. Therefore, patients during refeeding can develop gynecomastia.
5. Male hypogonadism. Gynecomastia occurs due to androgen deficiency.
a. Primary hypogonadism. It accounts for approximately 8% of gynecomastia cases. It can be due to a congenital abnormality such as Klinefelter syndrome, testosterone synthesis defects, or testicular defects (trauma, torsion, or infection)